An Investigation into Disaster Health Management in Saudi Arabia
Saeed Mohammed Alraga
DOI10.4172/2471-9781.100037
Ministry of Health Saudi Arabia, General Directorate of Asser Health Affairs, Saudi Arabia
- *Corresponding Author:
- Saeed Mohammed Alraga
Ministry of Health Saudi Arabia
Sarat Abiedah, Aseer
Saudi Arabia, MHM, Director Of Health Organization
Ministry of Health, Sarat Abiedah P.O. Box 240
61914, Sarat Abiedah, Aseer 61914, Saudi Arabia
Tel: +966503744473
E-mail: dr.alraga@gmail.com, salraga@moh.gov.sa
Received Date: August 21, 2017; Accepted Date: September 26, 2017; Published Date: October 25, 2017
Citation: Alraga SM (2017) An Investigation into Disaster Health Management in Saudi Arabia. J Hosp Med Manage. Vol. 3 No. 2:18
Abstract
The increasing occurrence of disasters around the world raises the issue of the effectiveness of a country’s crisis management systems, for example, the Kingdom of Saudi Arabia. Besides the potential damage and disruption to infrastructure, disasters can have a major effect on the health of a population. The direct consequences of a disaster are well known, i.e. deaths, injuries, disabilities and illnesses. Less well known are the indirect impacts on the overall health of a nation, in particular, its infrastructure, health systems, and service delivery. Such disasters can lead to long-term detrimental effects, namely, the erosion of social development and the loss of hard-won health and well-being gains. Therefore, there is a need for health to be a crucial consideration in disaster management. The current study sought to assess the Kingdom of Saudi Arabia’s (KSA) disaster health management system, with a focus on an examination of the intersection between healthcare and disaster management in the country. This investigation utilizes the (DHM) by utilizing the Disaster Health Management (DHM) model, developed by the World Health Organization (WHO). The findings show that, despite the number of disasters that have already occurred, the KSA does not have a multi-sectoral state department endeavor that facilitates effective disaster health management. Instead, the KSA continues to take a traditional health approach in relation to their response to emergencies and disasters. The critical findings regarding the DHM in the KSA, as well as the recommendations for further research, are provided for improving the current system.
Keywords
Disaster health management; World health organization; Primary health care; Emergency management services
Abbreviations
DHM: Disaster Healthcare Management; EMS: Emergency Management Services; GDCD: General Directorate of Civil Defence; KSA: Kingdom of Saudi Arabia; MODA: Ministry of Defence and Aviation; PHC: Primary Health Care; PPRR: Prevention, Preparedness, Responsiveness, Recovery; SARS: Severe acute respiratory syndrome; UNISDR: United Nations International Strategy for Disaster Reduction; WHO: World Health Organization
Introduction
Research background and rationale
Natural and man-made disasters are global concerns that can potentially kill, displace, and harm populations; disrupt health systems; deplete food, water, and energy supplies; bring down economies, and lead to massive infrastructural destruction. The United Nations International Strategy for Disaster Reduction’ (UNISDR) and the World Health Organization (WHO) define the term ‘disaster’ as “a serious disruption of the functioning of a community or a society” that leads to pervasive “human, material, economic or environmental losses which exceed the ability of the affected community or society to cope using its own resources” (World Health Organization (WHO) [1].
Disasters also refer to any spatial or geographical events in which an external stressor adversely impacts a human community, thereby carrying the implicit notion of non-manageability within a local context (Dar, Buckley, Rokadiya, Huda and Abrahams) [2]. It cannot be emphasized enough that disasters negatively affect the health, including the mental health, of individuals and communities, both directly and indirectly [3-5].
The direct impact of a disaster can include death, injury, disability, and illness, while the indirect health effects encompass damage to infrastructure, health systems, and service delivery. Apart from these effects, the adverse economic effects of disasters usually lead to an erosion of social development, as well as loss of hard-won health and wellbeing gains (Zahan, et al.). The detrimental health effects of disasters have been substantiated by many studies; however, the prevention or mitigation of these health effects represents a key challenge in terms of disaster prevention, preparedness, and health management.
The nature of health disasters in Saudi Arabia
The Kingdom of Saudi Arabia (KSA) has experienced a number of general health disasters as a result of overcrowding, terrorist attacks, and natural disasters (Abosuliman, Kumar and Alam). The most frequent occurrences of natural disasters in the KSA are in the form of flooding due to the fact that the country lacks a comprehensive drainage system (Abosuliman, et al.). When there are floods, families are not only displaced; they also suffer from adverse health effects as a result of waterborne diseases that get carried by floodwaters into the streets and then into their homes. Their health could be negatively impacted, especially the more vulnerable members of the population, such as the children and the elderly. Between 2000 and 2011, seven of the 11 most harmful natural disasters in the history of the KSA were caused by flooding (Alshehri, et al.). There are various reasons why flooding is a perennial threat to the KSA. The KSA is situated in a desert region where rain is a relatively rare occurrence. As a result, the drainage system in the country is underdeveloped and cannot cope in the event flooding rains [6]. Also, cities such as Jeddah and Makkah are situated in low-lying areas, surrounded by mountains. When rain falls in the mountainous areas, the water flows into valleys to eventually move toward these cities. Because of the poor drainage systems, this continuous flow of water usually leads to flash floods [6]. Hence, floods are considered major disasters in the KSA because they disrupt the normal lives of citizens, while business and government establishments cannot operate because of high waters. Therefore, floods tend to lead to personal, business, and national losses.
The KSA is also vulnerable to several hazard-oriented risks related to oil exploration and production activities in the country’s oil and gas sector (Al-Qahtani). These risks include oil leakages and spills, accidents in wells, fires, and explosions. When any of these risks occur, there are always adverse health effects. For example, oil seeps into water sources or toxic gases are spread in the air, and these can affect nearby communities.
While the magnitude and impact of the KSA disasters are not at the same level as those in other countries, their occurrences have increased in recent years. Heavy storms, for instance, due to the changing climate, have increasingly affected Saudi Arabia. This means that people may no longer be exposed only to minimal health hazards but also to health hazards of greater magnitude.
Another common type of disaster (i.e., a general health hazard) occurs in the KSA during the Hajj, an Islamic observance in which Muslims from different parts of the world go on a pilgrimage to the Holy Mosque in Makkah; this event takes place over five days in the 12th month of the Islamic calendar (i.e. either October or November in the Gregorian calendar). All adult Muslims, provided that they are physically and financially able to do so, are obliged to go on a Hajj at least once in their lifetime. During the Hajj season, Makkah’s population swells from 200,000 residents to more than three million people (Alshehri, et al.).
Therefore, the Hajj has been associated with increased risks of disasters that include mass trampling, food and water shortages and low health services that, in turn, have been linked to the spread of infectious diseases, as well as to other public health concerns. The Hajj has had a history of disasters that has led to many deaths and injuries. For instance, in 1990, 1,426 people were trampled in an overcrowded pedestrian tunnel leading to Makkah (Alshehri, et al.). In 2006, 346 people lost their lives due to overcrowding on the Jamarat Bridge in Mina, while tent fires have also killed hundreds of people. In light of these KSA disasters, the obvious need to evaluate the country’s disaster health management programs and systems cannot be overemphasized.
This study will identify and evaluate Saudi’s Health Disaster Management to determine the country’s readiness when the population faces risks to their lives and health.
Objectives of the Study
The current study seeks to evaluate the KSA’s disaster health management system. Specifically, it critically examines the intersection between healthcare and disaster management in the KSA. It is not unreasonable to believe that the KSA needs a Disaster Health Management Plan considering that it is located in a region where conflicts can arise. Further, as the current domestic healthcare system provides employment for thousands of foreign expatriates, it is a potential means of virus transmission that could impact the population. Fortunately, the KSA is a wealthy developed nation and therefore the funding considerations for the establishment of a comprehensive Disaster Healthcare Management Plan will not be a problem.
However, to achieve this outcome, this study must conduct two separate investigations: firstly, into the KSA’s healthcare, and secondly, into disaster management in the country. The purpose of investigating these two aspects is to determine if there is an effective integration of processes and systems that would enable effective disaster health management. There will also be a direct search for a Disaster Healthcare Management Plan and in the event that this plan is lacking, the paper will endeavour to present a way in which the health-care system can work with the disaster management team to develop a Disaster Healthcare Management Plan.
Research Questions
The current study seeks to address the following three research questions:
a. How effective is the performance of the KSA health-care system during a disaster?
b. How effective is the KSA’s disaster management system with specific reference to the way it integrates with the domestic health-care system?
c. What are the strengths and weaknesses of the current Disaster Health Management System in the KSA?
Significance of the Research
Disaster health management is rapidly becoming a unique specialty around the world, along with its theories and principles [7]. The disaster health management paradigm has four distinct elements (PPRR) that seek to improve the effectiveness of the disaster health response, namely: prevention and mitigation (P), preparation and planning (P), response and relief (R), and recovery (R) (Zhong, et al.). The overarching goal of disaster health management is to reduce the impact of disasters on human health and wellbeing through the provision of “urgent health interventions and ongoing healthcare during and after disasters” [7].
It is noteworthy that during disasters, the healthcare system becomes a high profile entity that plays a crucial role in society in terms of its immediate health response and the recovery phase. The system itself may be directly affected by disasters, yet is expected to continue to respond appropriately to consequent healthcare needs. To date, several studies have been undertaken on disaster risk management in KSA (e.g., Humphrey [8]; Al- Hasawi [9]; Al-Qahtani and Al-Dorzi [10]; Momani and Salmi [11]; Momani and Fadil [12]; Parker, Dunn, MacCall, Goetz, Park, Li and Koenig) [13].
However, the cited studies were not conducted in the context of disaster health management, but instead focused only on preparedness or emergency response. Other studies focused only on certain areas in the KSA. Hence, there is a dearth of knowledge in relation to the performance of KSA’s healthcare system during disasters, as well as the strengths and weaknesses of the current disaster health management system in the country. Therefore, the current study seeks to address this gap in literature. It is anticipated that the study’s results will provide insights into the workings of government agencies in KSA that are involved in disaster health management, and, in particular, how the policymakers, health and disaster risk management professionals work with the general public in the implementation of their roles.
Literature Review
A review of the existing literature was undertaken to determine which articles would best help answer the research questions. The main goal of the literature review was to assess the current theoretical and scientific knowledge regarding the phenomenon of disaster health management in Saudi Arabia [14]. Through the literature review, the researcher was able synthesize the information and data already known, and then determine what is unknown. A systematic and critical appraisal was undertaken of the most important and relevant literature regarding the phenomenon—disaster health management in KSA (McCourt et al.). Through examining the extant literature, the researcher gained an understanding of the current situation; from such a background, recommendations can be made in the event that there are systemic barriers against the creation of a comprehensive plan.
The following sections describe the literature search method, as well as the inclusion and exclusion criteria used in the selection of the studies being reviewed.
Literature search
According to Robinson and Reed [15], a literature review is “a systematic exploration of published work to find out what is already known about the intended research topic.” For a literature review to achieve its goal, the researcher should undertake a “systematic and explicit methodology to identify, select and critically evaluate relevant studies, and collect and analyse the data emerging from the studies included in it” [16].
It cannot be emphasized enough that the more knowledge researchers have about a given phenomenon, the better their understanding of it (Merriam).Thus, literature reviews seek to identify and analyse data that are specific to a phenomenon; however, they also strive to thoroughly comprehend the phenomenon and the forces that impact upon it. The current literature review on disaster health management in KSA was undertaken on papers and studies within the time frame of 2010 to 2015 only; this was to ensure that only relevant and recent research would be included in the review. The databases searched included: CINHAL Plus, MEDLINE, ProQuest, EBSCOhost, SAGE, Science Direct, and Wiley, as well as government websites.
The keywords used for this literature search were "disaster management plan + Saudi Arabia", “healthcare system + Saudi Arabia”, "health disaster management + Saudi Arabia", "health disasters + Saudi Arabia", among others. Other search terms were also used to unearth additional information that could be used to enhance the completeness of the study; for example, a search for “best practices in healthcare disaster management” that could be adapted for the KSA context. 49 of articles were identified in the original search. Inclusion and exclusion criteria were used to reduce this number, as described below.
Inclusion and exclusion criteria
Strict inclusion and exclusion criteria were used in the literature search to ensure that the study truly focused on disaster health management. The inclusion criteria stipulated that all articles were: (i) published in the English language; (ii) focused mainly on disaster health management in the KSA; (iii) involved empirical studies (qualitative or quantitative in nature) or theory-driven articles; and (iv) occurred in peer-reviewed journals or in other reputable sources.
The exclusion criteria were enforced if: (i) the full-text article had not been translated into English; (ii) the article had been published before 2010; (iii) the studies involved unethical practices, such as the use of human subjects for experimentation; and (iv) abstracts were in English, while the rest of the contents were in another language. From the original list of articles, using the inclusion and exclusion criteria, 11 articles remain. These articles were assessed and analyzed to determine the themes of the research, namely, the need for effective disaster health management, the nature of disasters, a disaster health model, and healthcare systems, multisectoral collaboration, and DHM priorities for action. They are discussed in detail in the following sections
The need for effective disaster health management
Complex and increasing threats to public health and safety drive the need for effective disaster health management; these threats include terrorism, biological disease outbreaks (such as Severe Acute Respiratory Syndrome (SARS)), and catastrophic natural disasters (such as hurricanes, earthquakes, tsunamis, and mud slides). The absence of a comprehensive disaster health management plan can lead to the loss of lives and the degradation of the health of many members of the population, both of which are preventable.
Notably, the potential for mass-casualty events, combined with the medical, political and public-safety issues associated with disasters, require that countries have effective disaster health management systems. For instance, studies show that countries ought to have skilled and experienced emergency responders who can efficiently respond to various types of events, and while doing so, can protect themselves, initiate command, communicate effectively, use technology, undertake timely triage and decontamination, as well as deliver medical care in and out of the traditional healthcare delivery venues.
However, a problem at hand is that even the most advanced countries may have inadequacies in appropriate disaster health management (Gordon, et al.). One probable reason for this is the lack of experience in the field. Hence, most countries are reactive in terms of responding to health disasters, such that they will only implement plans after something has occurred.
The nature of disasters
There are two types of disasters: natural, and technological or general. Natural disasters are naturally occurring physical phenomena that may result from rapid or slow onset events, namely: (i) geophysical, such as earthquakes, landslides, tsunamis, and volcanic activity; (ii) hydrological, such as avalanches and floods; (iii) climatological, including extreme temperatures, drought, and wildfires; (iv) meteorological, such as cyclones and storms; or (v) biological, such as disease epidemics and insect/ animal plagues (Zhong, et al.). At present, there are two health outbreaks that have the potential to affect the global arena. One is Ebola, which is concentrated in Africa, but can spread to other countries due to the movement of workers and visitors. The other one is the Middle East respiratory syndrome coronavirus (MERSCoV), which originated in the Middle East and has the potential of affecting a greater percentage of the population.
The second type of disaster is the technological or general type of disaster, comprising complex emergencies, conflicts, famine, displaced populations, industrial accidents, and transport accidents (IFRC). People cause these events, and they tend to occur in or near human settlements. Man-made disasters include “environmental degradation, pollution and accidents” (Button). One of the most destructive industrial accidents that impacted a whole nation and nearby regions was the Chernobyl disaster. This disaster had a great impact on health because of the nuclear elements that seeped into land and water, and because of noxious gases into the atmosphere.
The term ‘hazard’ refers to a perilous “phenomenon, substance, human activity or condition” that may lead to death, “injury or other health impacts, property damage, loss of livelihoods and services, social and economic disruption, or environmental damage” (UNISDR). The hazards that are most relevant to disaster health management are those with a natural origin and those associated with environmental and technological hazards, as well as risks. These hazards may be caused by different geological, meteorological, hydrological, oceanic, biological, and technological sources; they may sometimes work together (UNISDR).
However, what constitutes a risk? Risks pertain to the combined probability of an event and its negative consequences (Field). This means that risks may have the potential of becoming threats, and this applies to risks in the health sector. Despite the fact that risks exist and are real, any impact they might have on a population can be prevented or at least, minimized, if there is a health disaster management plan that could be implemented in a timely fashion.
The potential effect of a risk event on a society may be evaluated from another perspective besides the direct consequences of the event. Vulnerability pertains to the characteristics and circumstances of a community, a system or an asset that makes it susceptible to the adverse impact of a hazard or risk. There are different types of vulnerability with varying physical, social, economic, and environmental contexts. As an example, a structure’s physical vulnerability to hurricanes may result from poor design and construction, insufficient protection of assets, poor levels of public information and awareness, limited preparedness measures, and a disregard for prudent environmental management (Landesman and Weisfuse). Vulnerability dramatically differs within a given community and over time. As such, it is important for community members to determine what specific vulnerabilities exist in their communities and to establish how these may contribute to any perceived risk in the future.
Disaster health management model
As mentioned earlier, health is a crucial component of disaster management, as disasters directly impact the health of individuals, families, communities, and societies in general. Therefore, any government should always be prepared for eventualities that may impact upon the health not only of a few people but on a large number of the population. One recent public health issue facing the KSA nation is the MERS-CoV, a respiratory virus that is fatal for people if left untreated. Given this health threat, the country will need to have a plan in place so that the corona virus will be contained before it affects more people. In order to prevent its spread to a large number of people, the government should have a disaster health management plan that it can implement once health disasters are imminent.
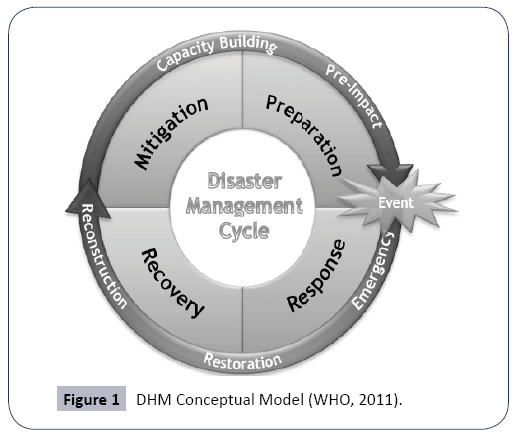
WHO (2012) asserts that a health system’s resilience and its capacity for emergency management, are crucial for effective disaster management [17]. Further, WHO (2011) posits that healthcare management should be integrated with disaster risk management and prevention in order to prevent deaths, injuries, diseases, disabilities, psychosocial problems and other health impacts. This integration results in a disaster health management (DHM) model which is multi-sectoral in nature. The DHM model will also serve as the conceptual framework for this paper. The model will facilitate the systematic analysis and management of health risks posed by emergencies and disasters, by means of: (i) hazard and vulnerability reduction for the prevention and mitigation of risks; (ii) preparedness; (ii) response; and (iv) recovery measures.
Figure 1 below depicts the cyclic DHM conceptual model: Importantly, one of the traditional thrusts of the health sector has been its response to emergencies. In this study, the challenge is to expand the focus of disaster risk management for health, from response and recovery to a more proactive approach, highlighting prevention and mitigation, as well as the development of community and country capacities for timely and effective response and recovery. According to WHO (2011), the development of resilient health systems, based on primary healthcare at the community level, can “reduce underlying vulnerability, protect health facilities and services, and scale-up the response to meet the wide-ranging health needs in disasters”.
The particular hazards addressed by the DHM are the natural disasters (i.e., earthquakes, landslides, tsunamis, cyclones, flood or droughts), biological disasters (i.e., epidemic diseases and infestations of pests), technological disasters (i.e., spills of chemical substance and radiological agents, as well as vehicular crashes), and societal hazards (i.e., armed conflict, stampedes, and acts of terrorism) that endanger entire populations, as well as imperil public health.
This study seeks to assess the Kingdom of Saudi Arabia’s (KSA) disaster health management system, with a focus on an examination of the intersection between healthcare and disaster management in the country. Disasters, emergencies, and other crises events can directly and catastrophically impact health and can indirectly impact facilities and services through the disruption of health systems especially during times when many do not have access to healthcare. These disasters can also impact upon basic infrastructure, such as water supplies and safe shelter, which are crucial for health. Therefore, the DHM model emphasizes the importance of its components, namely, healthcare systems and disaster risk management and prevention.
Healthcare systems
Based on the DHM model, healthcare systems serve as core capacities for disaster risk management of health (WHO, 2011). Notably, many countries have been struck by disasters, but if they have been without fundamental health services and infrastructure, they would have suffered disaster response difficulties. At the other end of the spectrum, those countries that have well-developed health systems are more resilient and better prepared and equipped to deal with disasters. Hence, essential healthcare system components for DHM include: primary healthcare; prioritization of community-based actions; hospitals and health infrastructure; and the development of adaptable and resilient healthcare systems are essential healthcare system components for DHM.
Firstly, primary healthcare (PHC) targets basic services for the improvement of health status that, in turn, strengthens community resilience and provides the basic foundation for emergency response. According to WHO’s (2011) DHM model, policies and strategies pertaining to PHC can reduce a community’s vulnerability by preparing households, communities and health systems for disasters. Usually, after a disaster, PHC focuses on acute care needs and specialist interventions. However, WHO (2011) emphasizes that, while these are important, what is more significant for DHM, are the remaining chronic and pre-existing conditions that convey the largest burden of disease.
Secondly, community-based actions are prioritized during disasters because these seek to protect health during emergencies. These community-based actions require: (i) local knowledge of local risks so that the real needs of the community are addressed; and (ii) local actions in terms of preventing risks at the source of the disaster through the provision on individuals’ exposure to local hazards (WHO, 2011).
Thirdly, hospitals and health infrastructure are of utmost importance in times of disaster. Health systems are comprised of public, private, and nongovernmental facilities that typically collaborate in delivering service to communities, and so these hospitals, primary healthcare centers, laboratories, pharmacies and blood banks help disaster-struck communities by ensuring, among other things, that the physical structures they occupy are sturdy, and therefore, in cases of emergencies, they can remain operational (WHO, 2011).
Finally, countries need to develop adaptable and resilient healthcare systems through the adoption of the following three approaches to emergency healthcare. In the first instance, they need to ensure they have adequate surge capacity to ensure that health systems can cope with large numbers of patients during disasters (WHO, 2011). Sometimes, this entails the mobilization of staff in different parts of the country in order to deliver services to the impacted areas. Next, they need to have flexibility in healthcare systems so that, through different functional departments, healthcare organizations can deliver a broad range of health services. Sometimes, this requires the reduction of certain services so that others may be increased. Finally, countries need to enact business continuity planning to ensure that healthcare facilities have established plans to guarantee that the health sector operates even in the midst of disasters. These contingencies include the identification of priority services and response frameworks that encompass coordination and communication with staff and partner organizations (WHO, 2011).
Multi-sectoral collaboration
For the purpose of protecting public health during and after a disaster, broader determinants of health (namely, water, sanitation, nutrition, and security) have to be sufficiently addressed through multi-sectoral collaboration (WHO, 2011). Critical infrastructure, including communications, logistics, and energy and water supplies, as well as emergency services and banking facilities, have to be safeguarded by means of multisectoral collaboration to ascertain continuity of health services.
DHM priorities for action
The WHO (2011) framework established five priorities for action to ensure that community and country resilience to disasters could be enhanced:
Priority 1: Disaster risk management for health should be a national and local priority. Therefore, to achieve this outcome, health and multi-sectoral policies, strategies and laws need to be developed and implemented for the purpose of providing direction and support for disaster health management, particularly at local levels (WHO, 2011). Apart from these aspects, coordination mechanisms need to be developed between the health sector and the multi-sectoral components, such as local and national governments. Thus, appropriate joint actions can be undertaken on risk reduction, and response and recovery by a variety of health and non-health actors. Governments and other stakeholders also need to collaborate and commit to the provision of adequate resources to support disaster risk management for health.
Priority 2: Healthcare systems need to undertake health risk assessments, as well as early warning mechanisms in the context of disasters (WHO, 2011). This entails the evaluation of risks to public health and healthcare systems, as well as the determination and implementation of risk management mechanisms, based on the said risk assessments. Efficient and effective surveillance and monitoring of potential threats to health are needed, particularly from biological and natural sources, to facilitate early detection and warning. These aspects would facilitate the timely action by the public, health workers, and other sectors.
Priority 3: Increased education campaigns, as well as the dissemination of information, are needed to contribute to the cultivation of a culture of health, safety and resilience at every level of society (WHO, 2011). Thus, through education, training and technical guidance, professionals from different disciplines would be able to increase their knowledge and skills, as well as to develop the appropriate mindset needed for the management of health risks implicated in disasters. Government agencies and the healthcare sector need to seek to inform and educate households and communities regarding disasters, so that they can prepare for, and reduce the risks related to these events. In this regard the media are important stakeholders, because they help disseminate accurate information pertaining to communitybased disaster health management programs in a timely manner.
Priority 4: Concerted efforts are needed to reduce “underlying risk factors to health and health systems” (WHO, 2011). This approach would encompass measures to reduce poverty so that the overall public health status could be improved. As a consequence, government agencies must ensure that: (i) new hospitals and healthcare centres are constructed with prescribed levels of protection; and (ii) current healthcare infrastructures are fortified so that they can continue operating and delivering healthcare services, even during disasters and emergencies. Therefore, government agencies need to take the lead in protecting critical infrastructure, with special attention given to facilities that have the potential to pose risks to public health, such as water and sanitation systems, chemical facilities, and energy sources. Such agencies also need to ensure that there is a strict compliance with building standards, regular upgrading or the retrofitting of health infrastructure, and the protection of ecosystems. There is also a need to monitor insurance regimes and microfinance programs in an attempt to ascertain that these businesses can continue operating across all healthcare settings.
Priority 5: Governments need to lead initiatives in disaster preparedness to enable an effective and efficient health response and recovery, at all levels, in the event of disasters. Such disaster preparedness covers “response planning, training, prepositioning of health supplies, development of surge capacity, and exercises for healthcare professionals and other emergency service personnel.”
Conceptual Framework
The methodology used in the current study, that is, the literature review approach, also served as the conceptual framework. The review was used to identify the major themes coming from the literature in disaster health management in the KSA. To determine these themes, three questions were developed and used.
Themes question from the literature review
This section outlines the themes from the literature review; they were identified using the following three questions:
a) How effective is the performance of the KSA’s healthcare system during a disaster?
b) How effective is the KSA’s disaster management system in the context of integration with healthcare management?
c) What are the strengths and weaknesses of the current disaster health management system in the KSA?
Disasters in Saudi Arabia
The KSA is vulnerable to a number of natural hazards, although to a lesser degree than many other countries. For instance, the north-western region of the KSA is prone to earthquakes and volcanic hazards, while the central and western regions of the country are vulnerable to floods [18]. Also, landslides are common in the inhabited mountainous regions of the southwest (Al-Basssam, et al.). Moreover, shifting sand dunes and dust storms are serious natural hazards that cities located in central and eastern KSA commonly encounter (Al-Basssam, et al.). In recent years, dust storms have become more common because of the expansion of cities, roads, and infrastructure development. Table 1 shows a summary of the disasters that have taken place in the KSA from 1941 to 2011, as well as the number of deaths and injuries that they caused (Abosuliman et al.).
Table 1: Disasters in KSA.
| Year | Type of disaster | Death | Injured |
|---|---|---|---|
| 1941 | Kabaa flash flood | N.A. | N.A. |
| 1964 | Flash Flood | 20 | 1000 |
| 1975 | Fire during Hajj | 200 | N.A. |
| 1979 | Occupation of Mosque in Makkah | 250 | 600 |
| 1985 | Floods in Northwest of Kingdom | 32 | 5000 |
| 1990 | Pilgrims Stampede inside tunnel | 1426 | N.A. |
| 1994 | Pilgrims Stampede inside tunnel | 270 | N.A. |
| 1997 | Yanbu and Asir floods | 26 | N.A. |
| 1977 | Fire during Hajj | 343 | 1555 |
| 2000/01 | Epidemic | 179 | 1700 |
| 2002 | Makkah floods | 31 | N.A. |
| 2005 | Medina floods | 29 | 43 |
| 2009 | Jeddah floods | 163 | 11640 |
| 2011 | Jeddah floods | 10 | 5000 |
Healthcare system in Saudi Arabia
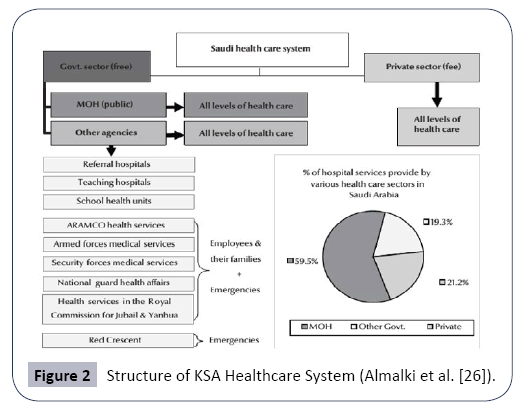
The KSA’s healthcare system ranks 26th out of 190 countries in the WHO (2000) World Health Report [19]. Notably, the KSA is a welfare state, with the Saudi constitution clearly stating that the government should deliver free healthcare services to all nationals (Albejaidi). Therefore, all Saudis have the right to free healthcare services, accessible in public healthcare facilities, in line with the government’s “Health for All” goal. However, there are also private providers of healthcare services who charge specific fees for their services. Both these public and private providers fall under the purview of the Ministry of Health (MOH) [20-24] which manages the KSA healthcare system.
The MOH is a “well-defined, decentralized organizational and administrative structure,” with functions that encompass “strategic planning, formulating specific health policies, supervising all health services delivery programs, as well as monitoring and controlling all other health-related activities” [25]. Preventive, curative, and rehabilitative healthcare are included in the free healthcare services provided for Saudis. The MOH provides roughly 59.5% of the health services in the Kingdom, free of charge, through 13 health directorates (Albejaidi). However, about 19.3% of the health service is delivered free through other government agencies, while the remaining 20% is provided by the non-government sector, which is growing rapidly.
Overall, the MOH delivers healthcare services by means of a network of primary healthcare centres that number 2,037, located in both large cities and small towns, and 244 hospitals [26]. Other government agencies that also provide healthcare services are the Ministry of Defence and Aviation (MODA), the Ministry of Education (MOE), the Saudi Arabian National Guard (SANG), the Ministry of the Interior (MOI), and the Red Crescent Society – all of which are independent of the MOH and have their own budgets for healthcare.
For instance, the General Department of Medical Services manages hospitals and primary healthcare centres under MODA. These public agencies provide healthcare services through different primary, secondary, and tertiary healthcare facilities for the benefit of their workers and their families. Aside from specialist hospitals, health facilities are designed to serve the workers of the different establishments and members of their families. Therefore, as a rule, these services are not available to members of adjoining communities and, in the event that these communities lack healthcare services, it is MOH’s duty to provide such services. The structure of the KSA healthcare system is presented in Figure 2 (Almalki, et al.).
Among the healthcare problems that need to be addressed by MOH and other government agencies are staffing shortages, financing and expenditure, evolving patterns of diseases, timely access to healthcare services, the introduction of a cooperative health insurance scheme, privatization of public hospitals, use of electronic health strategies, and the development of a national system for health information (Almalki, et al.).
Another emergent, pressing need for MOH and other government agencies is the development and implementation of practical plans and procedures to effectively manage disasters and crises. However, while hospitals and other healthcare facilities in KSA do have emergency response centres or departments, the DHM system itself does not appear to. Instead, the KSA seems to have fragmented initiatives pertaining to DHM; this topic is explored in more detail in the succeeding sections of this study. Nevertheless, it must be emphasized that disaster management is different from emergency management, although entities such as WHO (2002) and the United States’ Department of Homeland Security (DHS) (2015) [27] recommend that states adopt both approaches simultaneously. In summary then, a disaster is “a serious disruption of the functioning of a community or a society involving widespread human, material, economic or environmental losses and impacts, the ability of the affected community or society to cope using its own resources” (UNISDR). On the other hand, an emergency is “a state in which normal procedures are suspended and extra-ordinary measures are taken in order to avert a disaster” (WHO 2002) [28]. Both disasters and emergencies are addressed through the DHM model.
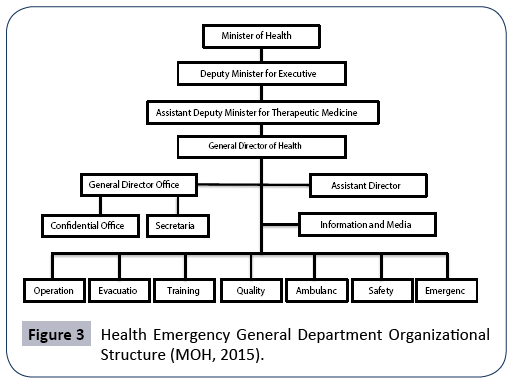
A number of studies [25,29] have shown that the KSA has paid little attention to developing a comprehensive approach to disaster management and response for the country. However, the KSA government has long shown a political willingness to adopt WHO’s DHM framework, as well as the Arab Strategy for Disaster Risk Reduction 2020 (Alshehri, et al.). The Council of Arab Ministers Responsible for the Environment (CAMRE) and the Socio-Economic Council of the League of Arab States, adopted the Strategy in 2011 and, by 2013, the Gulf Cooperation Council (GCC) had also taken proactive measures through the development of a risk reduction road map (Alshehri, et al.) [30]. Along with its commitment to participate in these initiatives, the KSA established the Health Emergency General Department under MOH (2015). The organizational structure of this Department is shown in Figure 3 below (MOH, 2015).This Department is led by the committee in charge of health contingency plans in the event of crises and disasters (MOH, 2015). Although this is a positive development for the citizens of KSA, according to the DHM framework, emergency response to disasters is not a fully sufficient public policy, as discussed in Chapter Two.
Meanwhile, Emergency Management Services (EMS) in the KSA has a long history. In 1965, King Faisal ordered the dissolution of the General Security and Fire Services so that it may be replaced by the General Directorate of Civil Defence (GDCD), under which EMS falls. Through the years, KSA’s experience of emergencies and disasters took their toll on the people and the country’s resources (Alamri). Because of the country’s extended geography, as well as being the destination of two important Islamic mass gatherings, EMS in the KSA has presented significant challenges which the GDCD has been striving to address. It is important to note that official policies regarding EMS are not easy to access, mainly because it falls under the GDCD and thus is considered a part of national security.
Nevertheless, the KSA has installed a new, comprehensive digital traffic control system in order to prevent multiple vehicular accidents and subsequent injuries and damages. This system is called the Saher, which translates to “watchful and napless” to imply its coverage of all roads within a city, 24 hours a day (Alamri). The Saher uses digital camera networks connected to the local command and control centre in every city that, in turn, are connected to emergency responders. Meanwhile, several projects and developments have been undertaken to make the Hajj process easier. Tunnels and sacred sites that have been the locations of stampedes now use one-way systems. Some sacred sites have been re-organized into floors to increase space efficiency as well as facilitate one-way travel.
Nevertheless, in Saudi Arabia, the efficiency and effectiveness of paramedics, emergency doctors and EMS administration require significant improvement [31]. Studies have shown that responders themselves admit that they require advanced training and experience in both basic and advanced life support procedures (Alanazi). According to a study conducted by Alanazi, even doctors in KSA are “seldom competent to decide on the need for emergencies, especially ventilation support, added oxygen, chest X-ray, airway selection” (Alanazi). It also appears that doctors and nurses in KSA have a low level of trust and confidence in EMS responders (Alanazi). The fault does not lie in the responders or their lack of training; however it has been found that doctors and nurses consider paramedics as nonclinicians who do not have adequate medical knowledge of the routines for patients in wards, ICUs and NICUs. For example, some paramedics have been found to have made mistakes in dealing with febrile seizure (Alanazi). Indeed, a number of doctors and nurses have voiced their doubts regarding the ability of paramedics to provide pre-hospital management (Alanazi). For example, a group of emergency physicians has been concerned about KSA paramedics’ inability to appropriately identify ST elevation myocardial infarction on ambiguous symptoms or ECG readings, resulting in valid cases being overlooked [31].
Paramedics in the KSA are also not permitted to “take independent decisions despite their being technically sound” (Alanazi). For instance, small children and infants do not need stretchers or ambulances when they are transported from a prehospital scene to the emergency department, unless there is a need for the equipment inside a regular ambulance. However, many paramedics in the KSA are not allowed to decide on the appropriate transport considering that non-ambulance transport cannot compromise in the system.
Additionally, emergency responders in the KSA commonly encounter resistance from patients, and such incidences of resistance constitute barriers to the effectiveness of the paramedics (Alanazi). Paramedics in the KSA also face numerous risks in delivering emergency care to children in the field, including legal issues that may arise from such care. Currently, paramedics in the KSA require training and advanced paediatric equipment so that risks may be reduced. Presently, emergency responders in the KSA believe that the general public and patients’ family members harbour low perceptions of their abilities. As an example, patients have complained about the punctuality of ambulance arrivals as well as about the inefficiency of paramedics’ interventions (Alanazi).
Disaster health management in Saudi Arabia
As discussed earlier, according to the DHM framework, disaster management for health considerations, should be a multi-sectoral endeavour, entailing the systematic analysis and management of health risks presented by emergency and disaster events (WHO, 2011) [32]. Therefore, the DHM model should promote a combination of prevention and mitigation, preparation and planning, response and relief, and recovery, known by its acronym, PPRR (WHO, 2011). Initial scrutiny of the KSA and the DHM model reveals that the country does not have such a multi-sectoral endeavour. Instead, the KSA appears to have a traditional health focus in relation to its response to emergencies. The following subsections describe PPRR in the context of the DHM.
Current practices in disaster preparedness
It cannot be emphasized enough that there is a dearth of empirical studies on DHM in the KSA. However, Abosuliman, Kumar and Alam [33] conducted an empirical study on disaster preparedness with a focus on the Jeddah flooding in 2009 and 2010. The participants in this study were representatives of the KSA, that is, decision makers and administrators who were accountable for disaster control in Jeddah (before, during, and after flooding in 2009 and 2010). The participants believed that, when it came to preparedness, response time was of primary interest, followed by efficiency, the cost structure, and the resources available. However, the study did not specifically disaster preparedness and what it entails. Typically, effective disaster response hinges upon adequate preparedness before the occurrence of any disaster (Zhong, et al.). The only empirical study addressing disaster preparedness in the context of the KSA’s healthcare system was conducted by Bajow and Alkhalil [34]; however, it focused only on six hospitals in Jeddah. Precautions to be taken to ensure that key indicators of disaster preparedness in hospitals, as identified by Bajow and Alkhalil [34], are met. They include: the location of the hospital structure, the architecture and furnishings, the safety of lifeline facilities, the maintenance of utilities, surge capacity, emergency and disaster plans, the control of communication and coordination and the structural vulnerability of proposed hospital buildings. The latter needs to be assessed through the use of hazard maps before being built to ensure that the hospital buildings are not at the edge of a slope or near the foot of a mountain, making it susceptible to landslides. At the micro level of planning, appropriate architecture and furnishings in hospital buildings also need to be effectively planned to minimize the effect of a disaster event. This includes windows, ceilings, partition walls, and lighting systems, as well as equipment (such as mechanical equipment, medicine containers, medical and laboratory equipment), and office furnishings, among others. The third indicator refers to the safety of lifeline facilities, which encompass electric power, water and sanitation, and waste treatment and disposal. All these factors play an important part in the continuous operations of a hospital and, consequently, need to be part of the special procedures and protocols for disaster preparation.
Moreover, the functional indicators of safe hospitals are of utmost importance during emergencies or disasters (Bajow and Alkhalil). Health services need to be available, especially in the midst, and after, disasters or emergencies. The location of the health facility is critical; it must be away from hazards, dust, noise, and fire. A hospital needs to be near proper roads with enough capacity for different forms of transportation. The maintenance of utilities should be excellent and there needs to be adequate water, as well as electricity and medical gas supplies. Hence, hospitals need to have a maintenance schedule that is followed strictly. ‘Surge capacity’ pertains to the capability of hospitals to increase their resources to meet a large casualty load without having to seek outside help; this capacity is considered important as it also incorporates the components of space, equipment, and staff.
As noted above, one of the most important components of surge capacity pertains to staffing, that is, doctors, nurses, mental health staff, emergency medical technicians, and public health professionals. A well-prepared hospital has specific benchmarks for surge capacity staffing and thus, needs a response system that allows for this surge capacity. Health professionals need to be trained in disaster preparedness through methods of competency-based education (Bajow and Alkhalil). Additionally, a hospital needs to have sufficient space so that it may be converted into patient facilities, such as when bed capacity has to be increased. Surge capacity also covers emergency plans for the supply of extra locations, food, and staff.
It cannot be emphasized enough that hospitals should have a Hospital Emergency Preparedness Response and Recovery Plan that is well-prepared and exercised (Bajow and Alkhalil). To this end, hospitals need to have hazard maps readily visible at all times, and emergency response leaders. Social workers or other professionals need to be prepared to disseminate public information and, preferably, a public information centre needs to be coordinated. The hospital’s disaster plan must cover the continued functioning of the public information centre during a disaster or emergency situation.
Communication is critical to the success of all coordination efforts, with hospitals needing to have access to pooled resources in the event that patients need to be transported. Therefore, hospitals need to have close coordination with local government agencies’ emergency plans as hospitals do not function in isolation during a disaster (Bajow and Alkhalil). Hence, it is important that emergency medical services (EMS) and hospital disaster plans are a part of the overall community disaster plan. Moreover, hospitals need to regularly update referral procedures to improve coordination with other hospitals and key disaster-related entities.
However, based on these indicators, it appears that disaster preparedness is much better in private hospitals in KSA compared to public hospitals. According to Bajow and Alkhalil, public hospitals and staff significantly lack training and management skills that can be implemented during a disaster. Other weaknesses include the lack of emergency and disaster plans, especially of hazard maps, as well as of information, committees, preparedness plans, hospital emergency incident command systems, emergency operations centres, and surveillance systems. Both private and public hospitals have shown a weakness in the control of communication and coordination. To further determine the exact nature of the current KSA situation, empirical studies on disaster preparedness are needed so that the Kingdom can better shift from its traditional focus on emergency responses.
The MOH site (2015) has published literature on its disaster preparedness measures. However, no empirical studies have tested the veracity of those findings or the potential liability of the implementation of these measures and activities. For instance, MOH (2015) established an Emergency Committee Health Central Directorate of Health Affairs (the Committee), which is in charge of health contingency plans in the event of crises and disasters. The Committee is in charge of developing rules and regulations, as well as of organizing the necessary arrangements that will enable MOH to adequately respond to emergencies, disasters and wars. The Committee also compels public and private hospitals to prepare for the eventuality of disasters. For instance, arrangements are made to ensure that there is a timely provision and transfer of the necessary amount of blood and plasma for blood banks, both public and private banks. Also, it is through the direction of the Committee that every healthcare facility has evacuation plans and takes measures to coordinate their activities with other healthcare entities.
Current practices in disaster prevention and mitigation
Significantly, disaster prevention in the KSA has improved considerably, especially in relation to disease-related hazards (MOH, 2015). MOH seeks to eradicate infectious diseases by continually upgrading the country’s surveillance system, and by insisting on the strict implementation of prevention and control programs. These continual efforts have led to the successful elimination of many infectious diseases. However, these are not the only considerations in disaster prevention. In terms of disaster prevention and mitigation, in the context of the DHM model, no single study has been undertaken in the KSA setting. Oftentimes, the terms mitigation and prevention are used as synonyms and interchangeably. WHO (1999) states that this is an acceptable practice because mitigation is encompassed in prevention. Nevertheless, the term mitigation refers to reducing “the severity of the human and material damage caused by the disaster”, while prevention seeks to “ensure that human action or natural phenomena do not result in disaster or emergency” (WHO, 1999) [35].
The primary goal of prevention is to avert, reduce or avoid the risk of an event occurring. This may be achieved by eliminating hazards or vulnerabilities, such as preventing overcrowding or deforestation, or providing services. WHO (1999) emphasizes that “healthier people in a healthy environment will be less vulnerable to most hazards”. Therefore, the KSA’s prevention efforts in terms of illnesses and epidemics are positive developments; for example, the immunization of citizens against smallpox has made them more resilient to the virus.
Moreover, disaster prevention and mitigation require the identification of threats and hazards as a first step towards managing their impact. Even when the hazard itself cannot be eliminated, vulnerability may be reduced in the case of a disaster event. Healthy communities and environments will have a greater and. stronger capacity to withstand, respond, and recover from disasters and emergencies. Healthier people in a healthy environment tend to be more capable of overcoming emergencies and disasters than others. Thus, the primary goal of mitigation is “to reduce the risk of being affected by a disaster” (WHO, 1999). Aside from the DHM model, the KSA is able to learn from the disaster prevention and mitigation strategy used in Canada.
However, to fully benefit from adopting aspects of the Canadian model, the MOH needs to take a leadership role, based the Canadian model, in managing mitigation and coordination (Public Safety Canada) [36]. MOH needs to spearhead collaboration across the board, as disaster mitigation activities typically involve all levels of government, the private sector, non-government organizations (NGOs), and communities. Collaboration and coordination among these entities are necessary to ensure an integrated approach to managing the mitigation. The second essential component of disaster prevention is partnership and shared responsibility. This is because the prevention of a disaster requires many experts who will come from different sectors of society. Therefore, disaster prevention should involve all levels of government, professional groups and academia, while the “private and voluntary sectors are encouraged to develop consensus on disaster mitigation matters” (Public Safety Canada). In the KSA, the participation of local stakeholder groups is the key to disaster prevention success.
Additionally, if MOH were to use the Canadian disaster prevention and mitigation strategy, it would need to initiate hazard identification and risk assessment; such actions would minimize the health impacts of probable disasters (Public Safety Canada). A concerted effort is needed to conduct risk assessments using methods such as historical research, data gathering, and “scientific estimations about hazard frequency, magnitude, damage potential, and vulnerability of potentially affected peoples and communities” (Public Safety Canada). Further, MOH needs to mobilize research, information dissemination, and decision support systems, as it is only through research that MOH will be able to gain useful insights into and tools upon which effective disaster mitigation decisions might be based. These approaches include risk assessment methodologies, land use practices, building engineering and best practices in public health protection.
Beside the Canadian strategy the Canadian strategy is the promotion of multidisciplinary public awareness, training, and education. Currently, the KSA appears not to have a culture of prevention and risk reduction. Such a culture may be achieved through sustained public awareness, training, and education programs which encourage government agencies, decision makers, and citizens to take into serious consideration, “the evolving threat and risk environment and the importance of implementing disaster mitigation measures” (Public Safety Canada). Before MOH can achieve a reduction in the risks due to hazards, there is a need to determine whether MOH perceives threats from other natural hazards, not only those related to floods. This determination is important as there seems to be an inordinate focus on flooding in the KSA, to the near exclusion of other natural hazards.
Lastly, and of utmost importance, MOH needs to initiate the development of incentives for disaster mitigation, especially if the latter is to become a priority among all stakeholders. Notably, the majority of mitigation implementation has to take place at the local level and necessitates up-front spending for future benefits to be achieved. This approach is not easy as such benefits can often be seen as too far in the future to have meaning. Nevertheless, it is important to emphasize that mitigation incentives must consider the need for “broad-based multi-level funding among all stakeholders” (Public Safety Canada).
Current practices in disaster response and relief
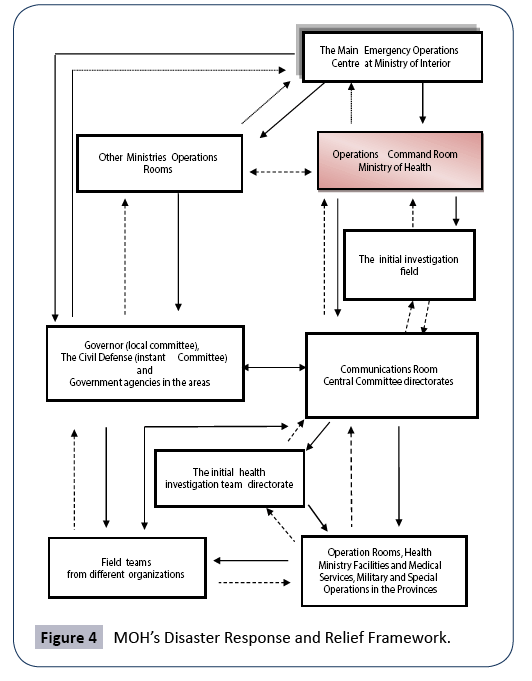
Today the KSA is most active in disaster and emergency response and relief, with MOH having developed a comprehensive framework in this regard (Figure 4). During disasters and emergencies, the MOH Committee evaluates and follows up on the events in order to assess how to best deal with them, especially in the context of health-related areas (MOH, 2014). The Committee then makes arrangements to ensure that the necessary workforce in the region is mobilized. Through the Committee, MOH provides medical supplies, equipment and ambulances, medicines and vaccines, and determines the health areas that are most affected. Preventive medical measures are then undertaken to prevent the further spread of the crisis or emergency. To this end, the Committee may authorize central laboratories to perform the necessary tests to help identify the threats of certain emergencies or threats. Moreover, the Committee coordinates with the government and private agencies from outside MOH to ensure that the overall response is adequate.
Current practices in disaster recovery
Currently, there is a dearth of empirical evidence regarding the KSA’s practices in disaster recovery. Therefore, this sub-section assesses the best practices in disaster recovery. According to Association of State and Territorial Health Officials (ASTHO) [37], planning for recovery can be successful only if it is undertaken before disasters and hazardous events occur. Recovery typically takes a long time and encompasses more complex activities than the response activities. Therefore, recovery needs to be an intentionally planned process that enables a community or country to define its own goals for recovery. One important primary rationale for post-disaster recovery is the establishment of a vision that serves as a guideline for decision makers, as well as a framework through which decisions can be taken.
One of the best practices of disaster recovery is to manage that recovery by goals and objectives rather than by activities, regardless of the cause. Four elements comprise this planning process: “goals, strategies, priorities, and criteria”. For instance, after a disaster, the KSA may decide that its recovery priority will be to help citizens return to their homes while, at the same time, maintaining access to healthcare for the most hard-hit of the population. This means that for every goal there needs to be a corresponding strategy detailing how the goal will be achieved. Usually before an event occurs, the goals and strategies need to be established. After the event, action steps need to be identified; these steps need to take into consideration the social, economic, and environmental conditions created by the disaster.
As resources for recovery tend to be limited, the goals need to be prioritized according to the pre-established criteria that integrate the possible condition or conditions of the community after the disaster, as well as the cultural values and politics (ASTHO). However, full recovery can only be achieved after all of the objectives have been achieved. As part of this process, clear response and recovery roles must be established, along with the clear identification of the decision-making authority, which should be the state health agency. Among the standard priorities of disaster recovery are the following six elements:
1. Restoration of health services and environmental safety to pre-event levels
2. Provision of long-term follow-up to citizens whose health has been affected
3. Implementation of recommendations from after-action reports following threats to public health
4. Restoration of health services and environmental safety to pre-event levels through the identification and implementation of recommended changes documented in the post-disaster evaluations
5. Ascertainment of ascertaining the sustained, fundamental and surge capacities of public health resources to “prevent, plan for, respond to, and recover from disasters” (ASTHO)
6. Attention to addressing the psychosocial needs of impacted populations, as well as the psychosocial needs of responders during and after an emergency (ASTHO).
Barriers to implementation of disaster health management
A country’s DHM plan can determine how many negative impacts are likely to take place. In the case of the KSA, multiple factors serve as barriers to an effective DHM system, most of which are social and demographic (Alamri). For instance, illiteracy and language barriers among vulnerable populations can prevent the effectiveness of a DHM strategy. These can also negatively affect citizens’ attitudes regarding emergency preparedness. In 2007, illiteracy rates in the KSA were 23.6% for females and 8.6% for males over 15 years old. These citizens will have great difficulty in reading and understanding DHM related materials and as a consequence, they could be more vulnerable to disasters. It must also be emphasized that the KSA uses the traditional approach to disasters, such that there is an inordinate focus on the emergency response. To ensure best practice for all community members affected by a disaster, it seems a useful suggestion that the KSA fully adopt WHO’s DHM model. Moreover, due to cultural forces, there is a tendency for Saudis to believe that disasters are God’s will and, thus, are inevitable (Alamri). However, this belief is contrary to Islamic teachings, which hold that every person has to endeavour to take precautions for their own safety and preparedness, aside from believing in God and relying on Him [38].
Recommendations
This study has highlighted the need for changes to KSA disaster management policies. Hence, it is recommended that the KSA adopt the five DHM priorities for action to enhance community and country resilience to disasters. These priorities are outlined below.
Priority 1
Disaster risk management for health needs to be a national and local priority (Schipper and Pelling). To achieve this outcome, health and multi-sectoral polices, strategies, and laws need to be developed and implemented for the purpose of providing direction and support for disaster health management, particularly at the local level (WHO, 2011). Additionally, coordination mechanisms need to be developed between the health sector and the multi-sectoral components, such as the local and national governments. This approach allows for joint action on risk reduction, response, and recovery by different health and non-health actors. Hence, governments and other stakeholders need to collaborate and commit to the provision of adequate resources to support disaster risk management for health.
Priority 2
The KSA healthcare system needs to undertake health risk assessments and develop early warning mechanisms in the context of disasters (Alshehri, et al.). Assessment will entail the evaluation of risks to public health and healthcare systems, as well as the determination and implementation of risk management mechanisms based on the said risk assessments. Additionally, efficient and effective surveillance and monitoring of potential threats to health are needed, particularly of those from biological and natural threat sources, in order to facilitate early detection and warnings (Landesman). These processes will lead to timely action by the public, health workers, and other sectors of society.
Priority 3
Increased education campaigns, along with the dissemination of information, would contribute to the cultivation of the culture of health, safety and resilience, at every level of society (WHO, 2011). Through education, training and technical guidance, professionals from different disciplines will be able to increase their knowledge and skills, as well as develop the appropriate mindset needed for the management of health risks implicated in disasters. Government agencies and the healthcare sector need to inform and educate households and communities regarding disasters so that they can prepare for, and reduce the risks related to disasters. Also, the media become important stakeholders in this regard; they can help in the timely dissemination of accurate information pertaining to community-based disaster health management programs.
Priority 4
Concerted efforts are also needed to reduce the “underlying risk factors to health and health systems” (WHO, 2011). Such efforts will encompass measures to reduce poverty so that the overall public health status will improve. Additionally, government agencies must ensure that: (i) new hospitals and healthcare centers are constructed with prescribed levels of protection; and (ii) current healthcare infrastructures are fortified so that they can continue operating and delivering healthcare services even during disasters and emergencies. Further, government agencies need to take the lead in protecting critical infrastructure, with special attention to facilities that can potentially pose risks to public health, such as water and sanitation systems, chemical facilities, and energy sources. It is important, therefore, that government agencies ensure strict compliance with building standards, the regular upgrading or retrofitting of health infrastructure, and the protection of ecosystems (Steelman et al.). There is also a need to monitor insurance regimes and microfinance programs to ensure that the businesses associated with these industries can continue to operate across all healthcare settings.
Priority 5
Governments need to be the leaders in initiating disaster preparedness because this will enable effective and efficient health responses and recovery, at all levels, in the event of disasters. Disaster preparedness covers “response planning, training, pre-positioning of health supplies, development of surge capacity, and exercises for healthcare professionals and other emergency service personnel” (WHO, 2011).
Conclusion
As determined in the current study, the KSA does not appear to be either well-prepared for natural disasters, or to be actively seeking to prevent disasters or emergencies. Additionally, the country does not seem to have clear mechanisms for disaster recovery. Despite these shortcomings, the KSA does have good disaster response measures. However, in terms of the health of a populace, these measures are simply not enough. Consequently, MOH, the department in charge of disaster activities in the Kingdom, needs to assess and consider the suitability of the WHO DHM model in order to develop a more comprehensive approach to disaster preparedness.
References
- (WHO) (2015) Definitions: Emergencies.
- Dar O, Buckley EJ, Rokadiya S, Huda Q, Abrahams J (2014) Integrating health into disaster risk reduction strategies: Key considerations for success. Ame J Pub Health 104: 1811-1816.
- Afifi W, Felix ED, Afifi TD (2012) The impact of uncertainty and communal coping on mental health following natural disasters. Anxiety, Stress & Coping 25: 329-347.
- Gerdin M, Clarke M, Allen C, Kayabu B, Summerskill W, et al. (2014) Optimal evidence in difficult settings: Improving health interventions and decision-making in disasters. Plos Med 11: 1-4.
- Zahran S, Peek L, Snodgrass JG, Weiler S, Hempel L (2011) Economics of disaster risk, social vulnerability, and mental health resilience. Risk Analysis: An Inter J 31: 1107-1119.
- Alamri YA (2012) Emergency management in Saudi Arabia: Past, present and future.
- Zhong S, Clark M, Hou X, Zang Y, FitzGerald F (2014) Progress and challenges of disaster health management in China: A scoping review. Global Health Action 7: 1-9.
- Humphrey J (1999) Casualty management: Scud missile attack, Dhahran, Saudi Arabia. Military Medicine164: 322-326.
- Al-Hasawi A (2008) Proposal on disaster management plan of Saudi Arabia based on earthquake damage estimation of Tabuk City. Bulletin InterInstSeismology Earthquake Eng42: 103-108.
- Al-Qahtani S, Al-Dorzi HM (2010) Rapid response systems in acute hospital care. Annals of Thoracic Medicine 5: 1-4.
- Momani NM, Fadil AS (2013) Risk management practices in the Saudi business organizations: A case study of the city of Jeddah. J Business Retail ManagRes7: 96-105.
- Momani NM, Salmi A (2012) Preparedness of schools in the Province of Jeddah to deal with earthquakes risks. Disaster Prevention & Management21: 463-473.
- Parker MW, Dunn LL, MacCall SL, Goetz J, Park N, et al. (2013) Helping to create an age-friendly city: A town & gown community engagement Project. Social Work & Christianity40: 422-445.
- McCourt R, Power J, Glackin M (2013) General Nurse’s experiences of end-of-life care in the acute hospital setting: A literature review. InterJ Palliative Nursing, 19: 510-516.
- Robinson D, Reed V (1998) The A-Z of social research jargon. New York: Ashgate. World Health Organization.
- Abalos E, Carroli G, Mackey ME, Bergel E (2006) Critical appraisal of systematic reviews: The WHO Reproductive Health Library, Geneva: The World Health Organization.
- World Health Organization (WHO) (2012) Health indicators of disaster risk management in the context of the Rio+20 UN Conference on Sustainable Development.
- Al-BassamAM, Zaidi FK, Hussein MT (2011) Natural hazards in Saudi Arabia.
- World Health Organization (WHO) (2000)The world health report 2000.
- Ministry of Finance (2014) Ministry of Finance statement about the national budget for 2014,Riyadh.
- Ministry of Health (2014)The new organizational structure of the Ministry of HealthMinistry of Health.
- Ministry of Health (2015) National e-health strategy. Ministry of health portal: Kingdom of Saudi Arabia.
- Ministry of Health (2015) Health statistics annual book. Jeddah: Kingdom of Saudi Arabia Ministry ofHealth.
- Ministry of Health (2015) Health emergency general department. Ministry of health portal: Kingdom of Saudi Arabia.
- Albejaidi FM (2010) Healthcare system in Saudi Arabia: An analysis of structure, total quality management and future challenges. J AlterPerspSociSci2: 794-818.
- Almalki M, Fitzgerald F, Clark M (2011) Healthcare system in Saudi Arabia: an overview. Eastern Mediterranean Health Journal 17: 784-93.
- Department of Homeland Security (DHS)(2015) Disaster response and recovery.
- World Health Organization (WHO) (2002) Disasters & emergencies.
- Al-Qahtani AM (2014) Disaster risks and preparedness: Effects of petrochemical hazards on the environment in Saudi Arabia. J EnviEarth Sci4: 129-139.
- Alshehri SA, Rezgui Y, Li H (2013) Public perception of the risk of disasters in a developing economy: The case of Saudi Arabia. National Hazards 65: 1813-1830.
- Alanazi AF (2012) Emergency medical services in Saudi Arabia: A study on the significance of paramedics and their experiences on barriers as inhibitors of their efficiency. InterJ ApplBasic MedRes2: 34-37.
- World Health Organization (WHO) (2011) Disaster risk management for health overview. Disaster Risk Management for Health Fact Sheets.
- Abosuliman SS, Kumar S, Alam F (2013) Disaster preparedness and management in Saudi Arabia: An empirical investigation. InterJ SocEduEcoManagEng7: 1972-1976.
- Bajow NA, Alkhalil SM (2014) Evaluation and Analysis of hospital disaster preparedness in Jeddah. Health 6: 2668-2687.
- World Health Organization (WHO) (1999) Overview: Disaster prevention & mitigation.
- Public Safety Canada (2014) National disaster mitigation strategy.
- Association of State and Territorial Health Officials (ASTHO) (2007) Disaster recovery for public health.
- Ministry of Economy and Planning (2013) The Saudi economy in figures 1434/1435H (2013G) Riyadh: Ministry of Economy & Planning.
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences