Community-based Preventive Interventions for Childhood Obesity: Design Strategies for Implementing a Population Health Management Program
Thomas TH Wan
DOI10.4172/2471-9781.100038
Public Affairs, Health Management & Informatics, and Medical Education College of Health and Public Affairs, Orlando, Florida
- *Corresponding Author:
- Thomas TH Wan
Professor of Public Affairs
Health Management & Informatics
and Medical Education College of Health
and Public Affairs, Box 163680
Orlando, Florida, USA
Tel: 407-823-3678
E-mail: Thomas.wan@ucf.edu
Received Date: September 11, 2017; Accepted Date: September 27, 2017; Published Date: October 25, 2017
Citation: Wan TTH (2017) Communitybased Preventive Interventions for Childhood Obesity: Design Strategies for Implementing a Population Health Management Program. J Hosp Med Manage Vol.3 No.2:19
Abstract
The statement of problem: The high prevalence of childhood obesity signifies a serious global health crisis. A systematic review on social and behavioural determinants of obesity reveals the complexity of childhood obesity and the need for comprehensive and innovative care management approaches at the population or community level.
Objective: This paper identifies a Trans disciplinary framework for integrating personal and societal determinants of childhood obesity and proposes the implementation of population health programs for obesity.
Approach: The pathogenesis of obesity is attributable to multiple factors. Thus, preventive efforts have to employ evidence-based implementation research to examine a complex set of etiologies and their relative influences on the outcomes of intervention programs. This investigation adopts a person-centered orientation coupled with the use of health information technology to design and evaluate care management programs for a target group of children at risk for metabolic disorders.
Implication: This prospective study design may generate workable care management plans targeting specific needs of obese children and enable us to yield useful information for expanding personal and social care models for population health management.
Conclusion: The longitudinal study of children served by community health centres may offer unique opportunities to provide practical information for enhancing the continuity of care and care management activities such as patient engagement management, risk identification and management, clinical case management, utilization management, and quality management of community services. Thus, optimal solutions to childhood obesity can be achieved by collaborative efforts of multi-sectorial partners such as academic, public health, private foundation, and community organizations.
Introduction
The high prevalence of childhood obesity signifies a serious global health crisis, particularly in rural and remote areas [1]. A systematic review on social and behavioral determinants of obesity reveals the complexity of childhood obesity and the need for comprehensive and innovative care management approaches at the population or community level [2]. Therefore, a population health management strategy to prevent and eradicate childhood obesity is suggested in this paper [3].
Age-specific research and development in pediatrics are lagging behind in preventive medicine [4]. This paper aims to design, evaluate and implement evidence-based preventive practices, including physical exercise, dietary education and other preventive activities for obesity, in a targeted group of children and teenagers in the Central Florida communities. The three-fold purpose of this study framed under a behavioral system model [5,6] coupled with contextual and environmental effects is to: 1) identify how integrated preventive interventions may influence the knowledge (K), motivation (M), attitude (A), and preventive practice improvement (P) and, in turn, affect health outcomes (O) of obese children who are identified by health professionals; 2) formulate and conduct a series of educational and training activities that enable health professional undergraduates to be engaged in service learning and practicum on childhood obesity prevention and intervention; and 3) establish a community-based network that shares the common interest in promoting and disseminating the best practices in reducing childhood obesity and preventive modules, using a health-educational technologybased decision support system for enhancing preventive behavior and practice in both rural and urban areas served by community health centers (CHCs) in Central Florida.
Related Research
Childhood obesity continues to be a major concern for public health officials, with current estimates at 17% of children aged 2-19 being obese [7]. In addition, Ogden et al. [7] report that Hispanics have a higher rate of obesity prevalence at 22.4%, as compared to black youth (20.2%) and white youth (14.1%). As children age, the prevalence increases with 8.4% of 2-5 year olds, 17.7% of 6-11 year olds and 20.5% of 12-19 year olds being obese. Body Mass Index (BMI) is the commonly used measure of obesity, with children in the 95% and above range being categorized as obese. Must and Tybor [8] discuss a BMI z-score, which incorporates 85% and above BMI scores, including age and gender. Of note, Mei, et al. [9] found that in the 2-19 year old age group, BMI for age was the best measure for detecting overweight in these children. In their conclusion for BMI, Mei et al. also considered skinfold thickness, as well as percentage body fat as determined by dual-energy x-ray absorptiometry, in their research.
Once a diagnosis of obesity has been established, management of the disease will require participation from several angles. Children look to parents and other authority figures for guidance in the management of variables such as portion size, dietary options and opportunities for exercise. Dietary intake and/or activity logs must be updated regularly with accurate data for tracking of progress. Children or their parents who are willing to actively and routinely provide this information are able to be a part of the wellness team. This active participation in the treatment plan can improve insight into obesity and its long term effects and solutions [10].
A distinct advantage of a treatment care plan is the ability it affords the child to be an active member of the team. Hopefully the child and family will seek to understand the concept of obesity. This understanding requires some level of health literacy by both the children and their parents. According to Ball, Smith, and Bakalar [11], a “dashboard” type tool allows participants to manage a disease and allows a case manager or clinician to provide an early intervention or support as needed. The dashboard can include level of activity in terms of what is accomplished on a daily or weekly basis.
If a formal exercise program is not followed, then at a minimum, active play time can be included. Children enjoy play time with their peers, and prefer this to dietary controls as a way to control weight [12]. In addition, children like a variety of video games, and research has indicated there are benefits of active video games such as Wii games [13,14]. To learn more about nutrition and exercise, mobile device apps for educational purposes have been developed to teach children about the food pyramid and attributes of exercise. These options are ideal when outdoor activity is not possible due to weather, allergies or other environmental constraints. The ability to record activity via a dashboard in a phone app or a website provides the possibility for tracking and feedback over time. Providing a variety of alternatives may stimulate children and adolescents to continually add to the options for an active lifestyle.
Theoretical Framework
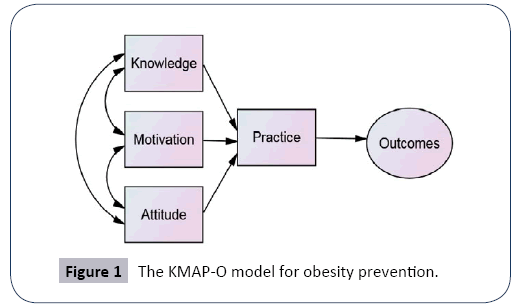
The research project is based on a behavioral system model [15,16] that consists of a transdisciplinary approach to the assessment of preventive intervention effects on the Knowledge- Motivation-Attitude-Practice-Outcome (KMAP-O) framework [5,17]. In the investigation of causal mechanisms of preventive interventions targeting a group of children who are likely to be susceptible to obesity and pre-morbid metabolic syndromes, we will employ this theoretically informed perspective guided by the logic model to assess program effectiveness. It is hypothesized that an integrated preventive approach to childhood obesity will directly affect children’s health knowledge, motivation to change, attitude toward guided behavioral intervention, and preventive practice as prescribed by health professionals and managed by case managers, and will indirectly influence outcomes of the participants via the improvement of knowledge, motivation, attitude, and preventive practice in the community health centres (Figure 1).
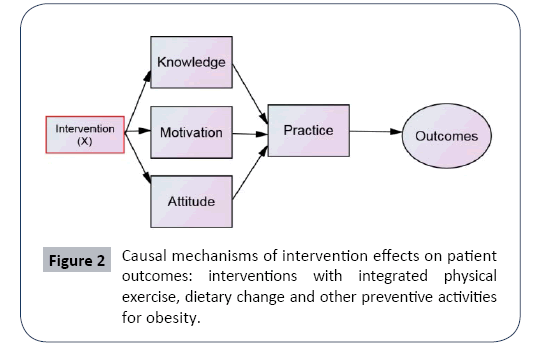
Based on a systematic review of scientific studies, researchers documented and highlighted the importance of varying interventions that will directly affect knowledge, motivation and attitude toward preventive practice. It is important to note that care management interventions should target the specific needs of children who are unable to adhere to specific prescribed preventive measures. Furthermore, care managers have to pay extra attention to the contextual, cultural and environmental factors that may mediate or intervene the relationship between KMA and P, as well as between KMAP and O. By integrating both personal and social determinants of childhood obesity, intervention programs can be formulated and implemented systematically. This is called a Trans disciplinary approach to obesity (Figure 2).
Specific research questions
1. Is there a standard set of assessment tools that are reliable, valid and applicable to the evaluation of an integrated preventive practice for childhood obesity reduction and better clinical outcomes?
2. What are specific components of the CHC-based physical and health education activities that will yield beneficial effects and better health outcomes for children who are obese and participate in CHC programs?
3. How can an integrated community-based preventive program for childhood obesity be effectively disseminated and diffused to multiple study sites in the Central Florida region as well as other geographic areas?
Methodology
Research design
A quasi-experimental study design is used to investigate how an integrated approach with physical exercise, dietary education and other preventive care activities will influence physical well-being and health related quality of life of obese children. A matched experimental and comparison groups of children who are referred by local physicians or clinics who agree to participate in the study will be selected, using the propensity score matching and analysis technique to avoid biased selection of the study subjects. The sample size is contingent up the number of intervention groups to be determined. The median effect size is assumed in this quasiexperiment. It is estimated that 200 individuals divided into the experimental and comparison groups will have enough power for testing the proposed model. Each study subject will be assessed six times during the two-year study period for each of the two cohort groups to generate baseline information in the first wave of the study, and follow-up assessments with repeated measures of specific KMAP-O indicators. Data generated from the first cohort study will be validated by the second-cohort study of 200 participants to determine the validity of the proposed KMAP-O model in preventive research.
The instruments selected for the study may include:
1. KMAP assessment: Preventive knowledge, motivation, attitudes toward prevention, and actual preventive practices such as objective measures of physical exercise with accelerometer, dietary consultations and other preventive activities will be assessed, using standardized scales and instruments that have demonstrable reliability and validity in the literature. Health literacy in age-specific groups of children must be assessed in the baseline evaluation [18].
2. Outcome assessment: A series of health-related outcome measures will be collected. They may include: 1) Paediatric Quality of Life Scale, 2) CES-Depression Scale, 3) BMI Scale, 4) physical fatigue, 5) self-perceived health, 6) adherence measures, 7) weight and height, and 8) metabolic and noninvasive measures of body composition.
3. Interventions: Three intervention strategies will be assessed and evaluated. They include physical exercise, dietary consultations, and health education activities.
Information will be gathered from a hand-held device to capture the data electronically [19]. Results from each wave of the study will be shared individually with the participants and families. When it is appropriate, assessment results will be shared with participants’ designated physicians. Analysis plan includes: 1) the intent-to-treat analysis with analysis of variance; 2) profile analysis of those who are most likely benefited from the integrated preventive program using predictor tree analysis; 3) latent growth curve modeling of determinants of the intervention outcome; and 4) impact analysis of the proposed researcheducation- extension program using logic model.
Education and training component
As a component of the integrated approach to childhood obesity and prevention, educational program and development will adhere four basic principles: 1) cultural sensitivity and responsiveness in the design of educational and training materials; 2) recognition of ethnic diversities in developing learning materials; 3) translation of manuals into multiple languages applicable to program participants; and 4) recruitment of pre-professional students in health sciences to serve as interns for service learning. Several educational modules will be designed and implemented: 1) Simulated learning to facilitate behavioral changes via information technology-based tools; 2) health educational products on nutrition and healthy eating with social media; 3) training modules for student interns who are engaged in service learning activities at the study sites; 4) on-line health educational courses for children and families participating in community health centers; and 5) preventive health briefs featuring benefits for engaging in physical exercises, dietary change, healthy food consumption, and other related preventive activities.
The collaborative research on childhood obesity and prevention with community health centers is to design research-educationextension projects to generate useful HIT-based decision support systems. The instructional technology, converting predictive analytics into useful GUI-based decision support systems, will be used. We will apply research results that identify the best intervention practices to the development of expert systems. Thus, based on the (KMAP-O) analytical model, we can develop a targeted approach to preventive interventions of childhood obesity. The decision support system is a game-based tool or app that can facilitate the decision process for engaging in preventive activities. In addition, an executive decision support system could be designed to aide providers or trainers in formulating care plans that will likely benefit the children. Training and application modules will be formulated to facilitate education and training activities associated with the proposed project.
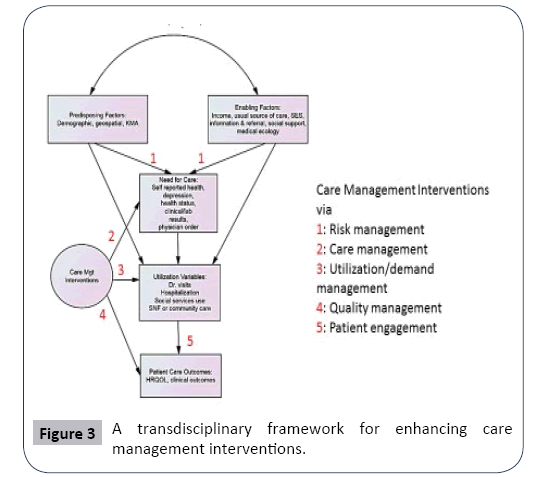
Care management component
The integrated approach to childhood obesity and prevention may consist of five managerial components, including 1) the risk management (identifying high-risk children for care), 2) the care plan and management (assessing needs and designing patientcentric care plans), 3) the utilization or demand management (profiling health services use and variability), 4) the quality management (assessing and tracking care outcomes), and 5) the patient engagement and management (offering health educational, motivational and adherence consultations). These managerial functions or activities can be seen from Figure 3. In addition, an extension component could be incorporated to function as a community extension network to diffuse new knowledge about the best preventive practices in obesity management or metabolic disease control. This integrated research-education-extension program is built upon the collaboration among four major organizations: 1) University of Central Florida with 62,000 students; 2) the Central Florida counties, including Marion, Sumter, Lake, Seminole, Orange, Osceola, Polk, Hardee, and Highlands; 3) CHCs enrolling a large number of people with multiple sites distributed in the 9 Central Florida counties; and 4) the local hospitals or children and family care centers serving children. The Central Florida CHCs have well-established social networks that include county extension stations and community-based organizations such as the YMCA.
Health information technology component
Information technology plays an important role in shaping health education and simulation. A variety of m-health or telehealth products can be used to formulate health education and intervention modules. For instance, a well-known health education and informatics product such as HealthyTutor (www.healthytutor.com) has been employed to improve health knowledge, motivation, attitude, preventive practice and outcomes of type-2 diabetes. For children and teenagers, we need to adapt this informatics technology to improve its readability and communicability, using a game-based approach to sharing educational materials and messages via a handheld device or cell phone. In addition, follow-up information should be captured via the cloud-based data collection system that can ensure the safety and security of the information gathered for program design and evaluation.
Implications and Conclusions
The proposed study is limited to its scope of work in the Central Florida CHCs. The project will formulate standard protocols for the diffusion and dissemination of educational materials prepared by the project team. The selected CHC sites will serve as the benchmark for coordinating extension activities. The generalizability of results may be limited to defined communities. However, the findings could yield multiple benefits for understanding the facilitators and barriers in the engagement or participation in physical exercise and other preventive activities of obese children. Thus, innovative strategies for enhancing adherence and engagement in health behavioral changes and preventive practices could be developed. Ultimately, the study will generate information to be incorporated into evidencebased practice in healthy community living.
The longitudinal study of children served by community health centers may offer unique opportunities to provide practical information for enhancing the continuity of care management activities such as risk identification and management, clinical case management, utilization management, and quality management of community services. Thus, optimal solutions to childhood obesity can be achieved by collaborative efforts of multi-sectorial partners such as academic, public health, private foundation, and community organizations.
References
- Karnik S, Kanekar A (2012) Childhood obesity: A global public health crisis. Inter J Preventive Med 3: 1-7.
- Kelshadi R, Aziz-Soleiman F (2014) Controlling childhood obesity: A systematic review. J Res Med Sci 19: 993-1008.
- Wan TTH (2017) Population Health Management for Poly Chronic Conditions: Evidence-Based Research Approaches. New York: Springer.
- Viergever RF, Rademaker CMA (2014) Finding better ways to fill gaps in paediatric health research. American Academy of Paediatrics 133: e824.
- Wan TTH, Terry A, McKee B, Kattan W (2017) A KMAP-O framework for care management research of patients with type-2 diabetes. The World J Diabetes 8: 165-171.
- Wan TTH (2017) A transdisciplinary approach to healthcare informatics research: Implications for poly chronic conditions. J Health Informatics Manag 1: 1.
- Ogden CL, Carroll MD, Kit BK, Flegal KM (2014) Prevalence of childhood and adult obesity in the United States, 2011-2012. J Ame Med Asso 311: 806-814.
- Must A, Tybor DJ (2005) Physical activity and sedentary behavior: a review of longitudinal studies of weight and adiposity in youth. Inter J Obesity 29: S84-S96.
- Mei Z, Grummer-Strawn LM, Pietrobelli A, Goulding A, Goran MI, et al. (2002) Validity of body mass index compared with other body-composition screening indexes for the assessment of body fatness in children and adolescents. Ame J clinical nutri 75: 978-985.
- Willis TA, Potrata B, Hunt C, Rudolf MCJ (2012) Training community practitioners to work more effectively with parents to prevent childhood obesity: the impact of HENRY upon Children’s Centres and their staff. J Human Nutr Diet 25: 460-468.
- Ball MJ, Carla Smith NCMN, Bakalar RS (2007) Personal health records: empowering consumers. J Healthcare Infor Manag 21: 77.
- Protudjer JLP, Marchessault G, Kozyrskyj AL, Becker AB (2010) Children's perceptions of healthful eating and physical activity. Can J Diet Pract Res 71: 19-23.
- Biddiss E, Irwin J (2010) Active video games to promote physical activity in children and youth: a systematic review. Arch Pediatr Adolesc Med 164: 664-672.
- Qualls KK, Arnold SH, McEwen IR, Jeffries LM (2013) Exercise Using the Wii Fit Plus with a Child with Primary Raynaud's Disease and Obesity: A Case Report. Phys Occup Ther Pediatr 33: 327-341.
- Andersen R, Newman J (1973) Societal and individual determinants of medical care utilization. Milbank Memorial Fund Quarterly 51: 95-124.
- Wan TTH, Soifer S (1974) Determinants of physician utilization: A causal analysis. J Health Soc Behav 15: 100-108.
- Ravmarathe K, Wan TTH, Marathe S (2016) The effect of health education on clinical and self-reported outcomes of diabetes in a medical practice. J Integrated Design Process Sci 20: 45-63.
- Sanders LM, Federico S, Klass P, Abrams MA, Dreyer B (2009) Literacy and child health: A systematic review. Arch Pediatr Adolesc Med 163: 131-140.
- Breen G, Wan TTH, Ortiz J (2010) Information technology adoption in rural health clinics: A theoretical analysis. J Inform Tech Impact 10: 1-14.
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences