An Economic Analysis of Using Scribes to Improve Hospitalists Workload
Hamzi A, Norman BA
DOI10.36648/2471-9781.20.6.253
Department of Industrial, Manufacturing & Systems Engineering, Texas Tech University, USA
- *Corresponding Author:
- Ahmed Hamzi
Department of Industrial, Manufacturing & Systems Engineering
Texas Tech University, USA
Tel: 312-241-3200
E-mail: Ahmed.hamzi@ttu.edu
Received Date: April 10, 2020; Accepted Date: April 27, 2020; Published Date: May 04, 2020
Citation: Hamzi A, Norman BA (2020) An Economic Analysis of Using Scribes to Improve Hospitalists’ Workload. J Hosp Med Manage Vol.6 No. 2:253.
Abstract
Hospitalists often experience the stress of high workloads. After the implementation of electronic healthcare record systems (EHRs), hospitalists on average spend 20% of their time documenting patients’ records in the EHR. One way to optimize hospitalist workloads is to partner them with scribes. This paper assesses how to economically justify having hospitalists work with scribes by taking into consideration many of the advantages of using a scribe in an inpatient setting.
Having scribes help manage patient records saves a significant amount of hospitalists’ time. Using data from the literature, four alternative approaches are considered to evaluate the financial impact of using scribes on hospitalists’ workload. A hospital needs to improve its case mix index (CMI) to help cover the cost of using scribes. Also, a hospital can reduce the number of hospitalists needed or increase admissions based on scribes improving hospitalists’ productivity. Additionally, considering scribes’ impact on hospitalists’ burnout reduces the required improvement in the CMI and admissions or the reduction in the number of hospitalists needed to offset scribes’ cost. Combinations of the approaches are also considered. Additionally, an Excel tool is developed to help decision makers in hospitals allocate hospitalists’ time savings and to assess the financial impact of scribes working with hospitalists for their context.
Scribes working with hospitalists can be cost justified in several ways as they help hospitals improve billing, reduce the number of hospitalists needed, facilitate increased admissions, and reduce hospitalist burnout.
Keywords
Scribes; Hospitalists; Workload; Cost
Introduction
Physicians spend a significant amount of their time on nonclinical tasks, such as administrative tasks, communications, and writing patients’ records into the electronic healthcare record system (EHR). Time consumed by these tasks limits the time physicians can dedicate to clinical tasks and direct patient care. The significant amount of time spent in the EHR burdens physicians as they prefer to spend their time on direct patient care. This affects the quality of care provided to patients, physician’s satisfaction, and patient’s satisfaction. Moreover, 70% of physicians think that EHRs reduce their productivity [1]. Scribes can ease the burden of writing patients’ records into the EHR, tracking orders and results, and prepare daily patient information for hospitalists, whose primary task is to provide general medical care to hospitalized patients, which results in hospitalist time savings and productivity improvement. Several studies in different medical settings show that scribes have positive impacts on physician and patient satisfaction. Scribes have been used more frequently in emergency departments and outpatient settings such as primary care and cardiology in comparison to the inpatient setting. In this paper, we evaluate cost justification methods for having scribes work with hospitalists.
Literature Review
Surveys show that the number of hospitalists is continuously increasing from slightly more than 10,000 in 2003 to more than 50,000 in 2016 [2], as a result of the more efficient inpatient care provided by hospitalists [3]. Hospitalists are responsible for both direct and indirect patient care, where they spend 18% of their time on direct patient care, and 69% on indirect patient care. Direct patient care includes taking the initial history and physical examination, seeing patients on subsequent days, and going over discharge instructions, while indirect patient care includes documentation, reviewing test results, creating medical records, and orders [4]. Hospitalists spend 34.1% of their time working with the EHR, and 58.4% of that time is used to write patients’ records into the EHR [5]. Therefore, about 20% (58.4%*34.1%) of hospitalists’ time is spent writing patients’ records into the EHR. In 2018, 56% of physicians indicated bureaucratic tasks as a contributing factor to burnout; 39% and 24% of physicians select too many hours at work and increasing computerization of their practice methods, respectively, as factors contributing to burnout [6].
A scribe may be an unlicensed, certified, or licensed person who provides documentation assistance to healthcare providers [7]. Scribes are often pre-medical students working closely with healthcare providers while they are in college or during their gap year. In the emergency department, it has been estimated that a physician with a scribe can see 0.8 additional patients per hour [8]. Also, physicians providing care to adult patients in the emergency department were able to produce an additional 0.2 relative value units (RVUs)/patient [9]. A study in a cardiology clinic shows that physicians with scribes saved on average 2.5 hours per day, which could be used to see about 10% more patients and complete documentation tasks within the workday [10]. Another study in a cardiology clinic shows that scribes improve patients seen per hour by 59% and work RVUs/hour by 57% [11].
A few papers consider the economic analysis of using scribes in the inpatient setting. A study done at two hospitals to measure the economic impact of scribes working with hospitalists found an improvement in the case mix index (CMI) by 0.28 in one hospital, and by 0.26 in the second hospital with revenue improvement of $12,000 per patient [12]. A group of hospitalists using scribes improved their daily census per hospitalist from 12-14 to 22-24 [13]. Scribes working with hospitalists also result in better documentation and improvement in patients’ records. At Paris Regional Medical Center, scribes reduced the need to call for locum tenens from six to eight times each month down to zero [14].
A study to measure the impact of scribes on primary care physicians ’ satisfaction shows that all the physicians were satisfied with the new workflow and 83% of the physicians with the use of the EHR after the implementation of the scribe system [15]. Another study shows that scribes have a significant improvement in all physician satisfaction factors, such as overall satisfaction with the clinic, and time spent with patients and patients’ records [16]. Family medicine physicians noted having better work-life balance after using scribes, particularly, when they were asked if their schedule provides them enough time to spend with their families. The impacts of scribes on hospitalists’ satisfaction and burnout needs further investigation; however, a hospitalist working with a scribe claims that scribes improve hospitalists’ productivity and worklife balance [14].
As previously mentioned, research about the use of scribes by hospitalists is limited. Thus, there is a need to assess the quantitative and qualitative benefits of using scribes by hospitalists to justify the cost of investing in scribes. In particular, from a purely financial perspective, the benefits of using scribes should be high enough to cover the costs associated with scribes. The objective of this paper is to show different approaches that can be used to economically justify using scribes in an inpatient setting.
Methods
This paper considers most of the benefits that scribes provide to hospitalists and quantifies them using different approaches to assess if scribes working with hospitalists is cost efficient. Data from the literature related to US hospitalists’ workloads and productivity have been used in this paper. We developed the Scribes Assisting Hospitalists Evaluation Tool that allows hospital decision makers to use their own hospital data in the economic analysis to obtain results that better reflect their own hospital’s particular circumstances.
Problem description
Hospitalists often experience the stress of high workload, especially after the adoption of EHRs. A recent Today ’ s Hospitalist survey shows that 61% of hospitalists find their workload is somewhat challenging, and 19% find it very challenging. Moreover, 53% of hospitalists find burnout a somewhat challenging issue, while 31% find it very challenging [17]. Consequences of burnout can lead to major issues such as lower quality patient care, medical errors, lower patient satisfaction, and hospitalist turnover which itself has consequences such as increasing workload for the remaining hospitalists and creating the need to search for new hospitalists which is both a costly and time consuming process. One way to optimize hospitalist workload and have them focus on direct patient care as well as reduce burnout related issues is to partner them with scribes. Thus, scribe benefits need to be quantified to justify the cost of hiring scribes to work with hospitalists.
Approaches
Hospitalists can save 20% of their time by having scribes write patient clinical information into the EHR. This paper considers four main alternative approaches to economically justify using scribes with hospitalists. In the first approach, the hospital improves its revenue by improving coding and billing and subsequently increasing its CMI, as a result of scribes helping produce more accurate and detailed patient records. In the second approach the hospital reduces the number of hospitalists needed by increasing the number of patients each hospitalist sees. The third approach increases admissions to the hospital. The fourth approach uses scribes to reduce hospitalist workload leading to a reduction in burnout and subsequent reduction in hospitalist turnover caused by burnout. Finally, combinations of these approaches are considered.
Costs of a hospitalist and a scribe
Hospitalists are a very expensive resource with an average annual compensation of $283,191 which includes salary, bonus, and incentive pay [17]. Family medicine and internal medicine hospitalists also usually get an additional 17%, and 14%, respectively, of their compensation as fringe benefits [18]. This means that hospitalist costs total $327,086 per year (assuming an additional 15.5% of their compensation is benefits). On the other hand, the average compensation of scribes is $13.29 per hour [19]. The total cost of hiring a scribe, considering benefits to be an additional 50% of their hourly rate [20] is about $42,365 annually.
Results
Approach 1: Generate additional revenue by using scribes
This approach evaluates offsetting the cost of scribes with the enhanced revenues that result from the CMI improvement due to the documentation work that scribes perform. Hospitalists at Saint Barnabas Medical Center in Livingston, New Jersey, report improvement in billing revenue postscribes. Also, in a pilot study Sound Physicians found that scribes help hospitalists to improve coding accuracy [13]. Scribes have also been shown to increase billing revenues in other medical contexts such as in a cardiology clinic [10] and in an emergency department [9].
In the inpatient setting, scribes help hospitalists to improve documenting patient records, which leads to improved billing and CMI as hospitalists can code more patients at higher diagnoses related groups (DRGs). Across the US, hospitals ’ base payment amount per patient for fiscal year 2019 was $6,105 ($5,646 for the operating base rate, and $459 for the capital rate) [21]. This means that each 0.1 unit improvement in the CMI will result in an additional revenue of $610.5 per patient (0.1*$6,105). The average geometric mean length of a hospital stay is 4.47 days [22]. On average, hospitalists work 15.4 shifts per month (184.8 days/year) with an average workload of 16.1 patients/shift [17].
The following calculation shows how much improvement is required in the CMI to offset the cost of scribes:
Number of discharges/year=(184.8 days/year × 16.1Beds)/ (4.47 Bed days/discharge)=666
Break Even point=(Scribe's cost)/(Number of discharges × Base amount)=$42,365/(666 × $6105)=0.0104
Therefore, a hospital only needs to improve its CMI by 0.0104 to cover the cost of scribes.
Approach 2: Reduce the number of hospitalists needed
This approach considers reducing the number of hospitalists needed per shift since the scribes reduce the hospitalists ’ workload. Consider the following hospitalist workload related data. The average length of a hospitalist’s shift is 11.5 hours and on average a hospitalist works 15.4 shifts per month [17]. Hospitalists spend 20% of their time writing into the EHR which represents about 2.3 hours per shift [5]. A different study to assess hospitalists’ activities shows that hospitalists spend 25.5% of their time on documentation which results in 2.9 hours per shift for an 11.5-hour shift [4]. According to expert opinion, hospitalists spend only 5 minutes reviewing discharge summaries produced by scribes, instead of spending 45 minutes on each discharge summary as was the case before the use of scribes [13]. In addition to the time saved from documentation, there are other tasks that scribes perform for hospitalists which will result in additional time savings, such as tracking orders and results, preparing patient lists for rounding, and gathering and preparing information for hospitalists. However, to be conservative, in this analysis only the time spent writing patients ’ records into the EHR is considered as time saved by the scribe, and this is assumed to be 2.3 hours during an 11.5-hour shift.
The 20% of hospitalists’ time saved by scribes can permit hospital management to reduce the number of required hospitalists by 20% and still serve the same number of patients. For example, if a hospital has 10 hospitalists who serve 161 patients in total (10 hospitalists*16.1 patients/ hospitalist), then the hospital needs 8 hospitalists to serve the 161 patients with the use of scribes as each hospitalist will be able to see 25% more patients. This will result in a reduction of $654,171 per year in hospitalist costs. However, hospitals only need a 10.36% reduction in the number of hospitalists needed in order to offset the cost of scribes.
Approach 3: Increase admissions to the hospital
This approach assumes that the hospital is not currently operating at full bed capacity. In this case, the hospital can use the time saved by scribes to increase the number of patients seen per hospitalist, allowing the hospital to more fully utilize bed capacity. The additional revenue generated by increasing admissions to the hospital by 25% is more than enough to offset scribe costs as a hospital only needs a 1.04% increase in admissions to breakeven.
Approach 4: Reduce hospitalists burnout
In this approach, the time saved by scribes is used to reduce hospitalist workload in order to reduce burnout, as high workload is one of the top factors causing physician burnout. Scribes not only help reduce this burnout contribution factor, scribes help on others too, such as performing bureaucratic tasks, which is the most important factor causing physicians’ burnout, and computerizing the practice using an EHR. One of the major financial costs related to hospitalists’ burnout is turnover cost. Studies show that burned out physicians are twice as likely to turnover as non-burned out physicians [23]. Given the fact that the hospitalist burnout rate is 52.3% [24], and the general hospitalists’ turnover rate is 6.9% [25], using Shanafelt’s approach to calculate the turnover rate due to burnout results in the following:
Turnover=[Turnover without burnout × (1-Burnout rate)] + [(2 × Turnover without burnout) × Burnout rate]
Solving for turnover without burnout:
Turnover without burnout=(Turnover)/(1+Burnout rate) Since the turnover rate consists of both turnover due to burnout and turnover without burnout, then:
Turnover rate due to burnout=turnover rate - ((turnover rate)/(1+burnout rate))
Turnover rate due to burnout=0.069 - (0.069/ (1+0.523))=2.37%
Therefore, 2.37% of the hospitalists’ turnover annually is a result of burnout.
The average time frame for hiring a new physician to fill a vacancy is 8 months [26]. However, most hospitals required a hospitalist to give notice 4 months before resigning. This gives hospital management a chance to start searching for a new candidate four months before the hospitalist leaves. Costs associated with sourcing, and interviews to hire a new physician are $41,090 for a 12 month vacancy and $47,598 for 6 month vacancy [27]. The recruiting process also typically includes a signing bonus of $30,000, moving costs of $15,000, and start-up for a new physician estimated at $211,063 [27]. Assuming that sourcing and interview costs are linear, then the sourcing cost for 8 months is $45,429. This results in a cost of $301,492 to hire a hospitalist within 8 months.
In the inpatient setting, most of the time the revenue loss due to hospitalist turnover is not considered, because the hospital will increase the workload of the remaining hospitalists or hire locum tenens to take care of the hospitalized patients. Hiring a locum tenens, paying extra compensation to the current hospitalists to take on the extra workload, and providing no extra compensation are the options that are considered in this analysis with the assumption that extra compensation is equal to the average hospitalist’s compensation without benefits. The cost of hiring a locum tenens is $437,035 per year [28]. Note that $109,029 of the hospitalist salary is saved by the position being vacant for four months. Thus, total turnover cost is $338,141, $286,860, and $192,463 for the locum tenens, extra and no extra compensation options, respectively.
Considering a hospital with 10 hospitalists, then the expected number of hospitalists that turnover as result of burnout is 0.237 hospitalist per year with an expected cost of $80,122, $67,971, and $45,604 for the cases of hiring locum tenens, extra compensation, and no extra compensation, respectively. Therefore, considering this approach alone does not economically justify providing scribes for hospitalists.
Combinations of the approaches
We now consider combinations of the approaches mentioned previously where benefits of real time documentation and improvement in the CMI by using scribes can readily be combined with the benefits of the other approaches to justify scribe costs.
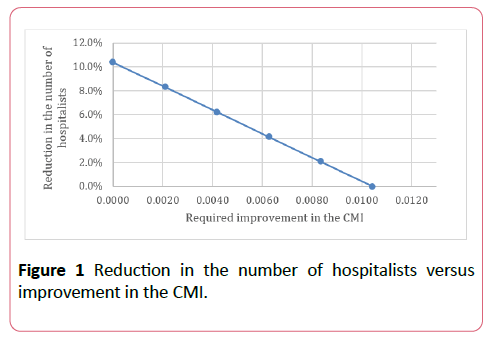
Approaches 1 and 2: In this approach the additional revenue from the CMI improvement and the cost savings from reducing the number of hospitalists are considered. The hospital can reduce the number of required hospitalists by less than the breakeven point which is 10.36%, and still offset scribe costs, if approach 1 is considered. Figure 1 shows the relationship between the reduction in the number of hospitalists needed and the required improvement in the CMI to pay for scribes. All areas on the graph at or above the line indicate that scribes are financially beneficial.
Approaches 1 and 3: This approach considers both the additional revenue from the CMI improvement and revenue from an increase in hospital admissions to offset scribe costs. Hospitals that are not running at full bed capacity can increase their admissions by less than the breakeven point of 1.04% and still cover scribe costs if the additional revenue generated from the CMI improvement is considered. For each increase in the CMI of 0.002 the breakeven point for the increase in admissions reduces by about 0.2%. Thus, a hospital could consider both approaches to offset scribe costs. Since most hospitals would have other constraints that would limit the potential to increase admissions, approach 3 is only considered in combination with approach 1 in the paper. However, the Scribes Assisting Hospitalists Evaluation Tool allows the user to consider other combinations.
Approaches 1 and 4: Considering the expected cost savings from reducing the burnout rate and increased revenue from CMI improvement, a hospital needs less improvement in the CMI than when considering approach 1 alone to offset scribe costs with a required CMI improvement of 0.0085, 0.0088, and 0.0093 for the locum tenens, extra compensation, and no extra compensation options, respectively.
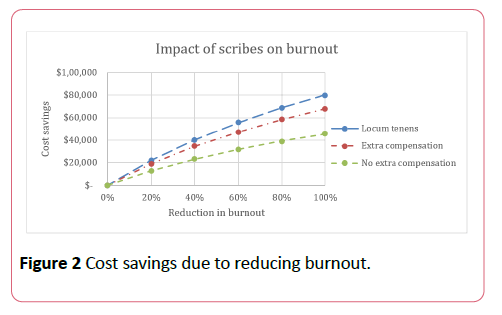
These results assume that scribes will eliminate all burnout factors, which may not always be true, although scribes help to reduce burnout coming from the most important factors contributing to hospitalist burnout. Figure 2 shows the effects of different percentages of burnout reduction. Table 1 shows the required improvement in the CMI to offset scribe costs for the combination of approaches 1 and 4.
Table 1 Required improvement in CMI to offset scribe costs with burnout reduction.
| Burnout reduction | Required improvement in CMI | ||
|---|---|---|---|
| Locum tenens | Extra compensation | Noextra compensation | |
| 100% | 0.0085 | 0.0088 | 0.0093 |
| 80% | 0.0087 | 0.009 | 0.0095 |
| 60% | 0.0091 | 0.0093 | 0.0096 |
| 40% | 0.0094 | 0.0096 | 0.0099 |
| 20% | 0.0099 | 0.01 | 0.0101 |
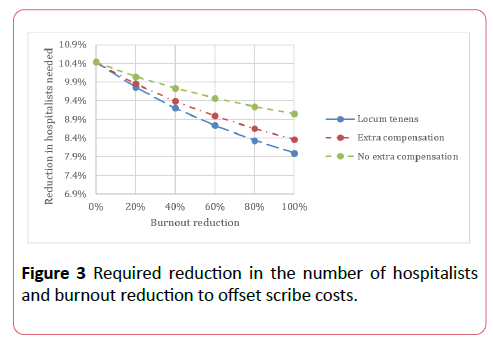
Approaches 2 and 4: Having scribes working with hospitalists significantly reduces the time that hospitalists spend with the EHR and subsequently reduces hospitalist burnout. Scribes also help hospitalists with some bureaucratic tasks, which will positively impact hospitalist satisfaction even with an increase in hospitalist patient workloads, as hospitalists prefer to spend their time on direct patient care. In this approach, the combination of the reduction in the number of hospitalists needed and the savings from the reduction in hospitalist burnout are considered to offset scribe costs as shown in Figure 3.
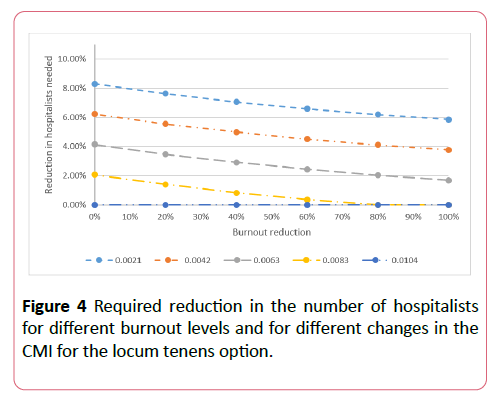
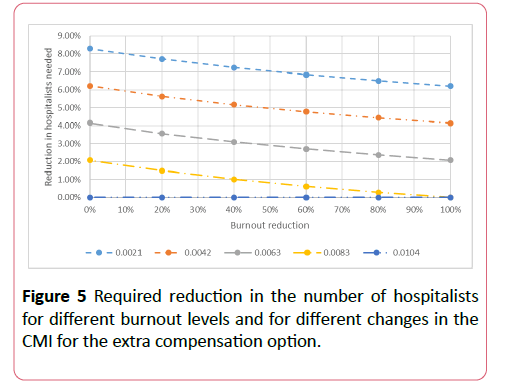
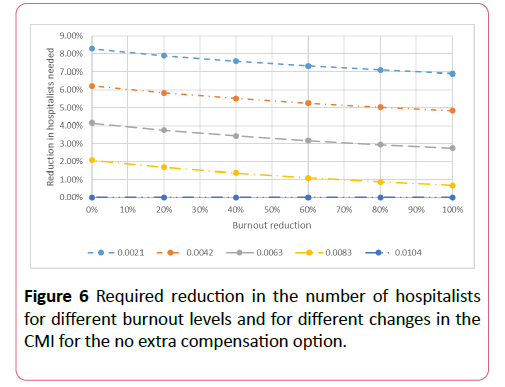
Approaches 1, 2, and 4: In addition to the reduction in hospitalist burnout, scribes also help hospitals to generate more revenue due to the improvement in the CMI as mentioned in approach 1. Figures 4-6 show the required reduction in the number of hospitalists to offset scribe costs for different hospitalist ’ s vacancy options for CMI improvement values ranging from 0.0021 to 0.0104.
Excel tool
An Excel tool has been developed to assist hospital decision makers with assessing the impact of allocating hospitalists’ time savings across the four different approaches considered above based on their preferences and other factors unique to their particular hospital’s situation. This way decision makers can make a data driven decision on how to cost justify hiring scribes that reflects their key cost considerations. (See Scribes Assisting Hospitalists Evaluation Tool, Supplemental Digital Content 1, to explore the Excel tool).
Discussion
In addition to the greater revenue generated by having more accurate patient records and subsequently improving the CMI, reducing the number of required hospitalists, increasing admissions to the hospital, and reducing hospitalists burnout are possible approaches to justify scribe costs.
For the approach of increasing hospital admissions, the decision to increase admissions is dependent on other factors such as having beds available and sufficient staff and other related resources. In the fourth approach, the cost of hospitalist turnover depends on the hospital ’ s strategy for dealing with a hospitalist position vacancy. However, high workload, work-life balance issues, and hospitalists’ burnout are some disadvantages associated with the paying and not paying extra compensation options. In the event of hospitalist staffing shortages due to turnover, hospitals may reduce their admissions, but this would lead to revenue loss which would be highly undesirable. Therefore, hiring scribes is likely to be a cost effective alternative.
It is important to note that in this paper the only time savings considered is the time that scribes save for hospitalists by taking responsibility for writing patient records into the EHR. But there are other administrative tasks that scribes can do for hospitalists such as documenting prescription and discharge instructions, coordinating follow up calls, and communicating with patients. If all of these factors were considered, the cost savings from using scribes would be even greater.
There are some important limitations to consider regarding this analysis. Introducing scribes to provide documentation assistance to hospitalists requires effort from all stakeholders to facilitate the implementation of the scribe program. Particularly, providers and scribes need to communicate and agree on the format of the patient record and what is to be included in it [29]. It may take some time for scribes to reach their target level of productivity, but this generally only requires a few months [30]. A scribe may only stay at a hospital for a short period of time and therefore the issue of high turnover among scribes is important to consider [31]. Hospitals may need to develop career paths for scribes to minimize the turnover rate and improve scribe practices in the hospital.
As previously mentioned, scribes can perform other tasks in addition to documentation. Thus, the actual monetary benefits of having scribes working with hospitalists needs to be thoroughly investigated and ideally piloted to have a comprehensive view of scribes’ benefits. Finally, in order for a hospital to maximize the benefits coming from using scribes, the optimum number of scribes to hire needs to be determined with consideration of uncertainty in scribe attendance.
Conclusions
Hospitalists with scribes can see more patients, submit more accurate billing, and improve workflow by entering orders and documentation sooner in the day. In addition to the improvement in the CMI, hospitals can justify scribe costs by the following: reducing the number of required hospitalists, increasing admissions (if the hospital is not running at full bed capacity), and reducing hospitalist workload to reduce burnout and turnover cost, although this approach in isolation does not offset the full cost of scribes. Having hospitalists work with scribes can be economically justified by considering the above approaches in isolation or in different combinations. Considering each approach separately may underestimate the actual value of scribes. Therefore, this paper considers different combinations of approaches to represent the actual value that scribes bring when working with hospitalists.
Providing hospital decision makers with an easy tool to assess the cost effectiveness of having hospitalists work with scribes could facilitate the process of establishing a scribe program in an inpatient setting. The Excel tool that we developed, provides a user friendly format to utilize some of the information presented in this paper to cost justify hospitalists working with scribes, and to assess the impact of different allocations of the resulting time savings on the cost effectiveness analysis.
In addition to the quantitative advantages of having scribes working with hospitalists, scribes can have qualitative advantages. One of the advantages is improving patient satisfaction, as hospitalists will be able to have more face to face interaction with patients due to there being less need to spend time in the EHR. Scribes also have a significant positive impact on hospitalist job satisfaction and work-life balance as scribes help hospitalists to focus more on patient care and less on the EHR, as well as to avoid after hours documentation tasks.
References
- Deloitte (2016) Survey of US Physicians Findings on health information technology and electronic health records.
- Wachter RM, Goldman L (2016) Zero to 50,000 The 20th Anniversary of the Hospitalist. N Engl J Med 375:1009-1011.
- Elliott DJ, Young R, Brice J, Aguiar R, Kolm P (2014 Effect of Hospitalist Workload on the Quality and Efficiency of Care. JAMA Intern Med 17:786-793.
- O'Leary KJ, Liebovitz DM, Baker DW (2006) How hospitalists spend their time: Insights on efficiency and safety. J Hosp Med 2:88-93.
- Tipping MD, Forth VE, O'Leary KJ, Malkenson DM, Magill DB, et al. (2010 Where did the day go? A time‐motion study of hospitalists. J Hosp Med 6:323-328.
- Medscape (2018) National Physician Burnout & Depression Report.
- The Joint Commission (2018) Documentation Assistance Provided By Scribes.
- Arya R, Salovich DM, Ohman-Strickland P, Merlin MA (2010) Impact of Scribes on Performance Indicators in the Emergency Department Rajiv. Academic Emergency Medicine 17:490-494.
- Heaton H, Nestler D, Jones D, Varghese R, Lohse C, et al. (2016) Impact of Scribes on Billed Relative Value Units in an Academic Emergency Department. Annals of Emergency Medicine 68.
- Bank AJ, Gage RM (2015) Annual impact of scribes on physician productivity and revenue in a cardiology clinic. ClinicoEconomics and outcomes research: CEOR 7: 489-495.
- Bank AJ, Obetz C, Konrardy A, Khan A, Pillai KM, et al. (2013) Impact of scribes on patient interaction, productivity, and revenue in a cardiology clinic: a prospective study. ClinicoEconomics and outcomes research: CEOR 5:399-406.
- Kreamer J, Rosen B, Susie-Lattner D, Baker R (2015) The economic impact of medical scribes in hospital. Physician Leadersh J 2:38-41.
- Darves B (2014) Scribes: the solution for too much paperwork. Today’s Hospitalist.
- Gesensway D (2018) Is there a scribe in your future? Weighing the pros and cons. Today’s Hospitalist.
- Pozdnyakova A, Laiteerapong N, Volerman A, Feld LD, Wan W, et al. (2018) Impact of Medical Scribes on Physician and Patient Satisfaction in Primary Care. Journal of general internal medicine 33:1109-1115.
- Gidwani R, Nguyen C, Kofoed A, Carragee C, Rydel T, et al. (2017) Impact of Scribes on Physician Satisfaction, Patient Satisfaction, and Charting Efficiency: A Randomized Controlled Trial. Annals of family medicine 15:427-433.
- https://www.todayshospitalist.com/survey/17_salary_survey/b01.php
- American Medical Group Association (2015) Medical Group Compensation and Productivity Survey.
- https://www.indeed.com/q-Medical-Scribe-jobs.html
- U.S. Bureau Of Labor Statistics (2019) Employer Costs for Employee Compensation.
- Medicare Payment Advisory Commission (2018) Hospital acute inpatient services payment system.
- https://www.cms.gov/Medicare/Medicare-Fee-for-Service-Payment/AcuteInpatientPPS/FY2018-IPPS-Final-Rule-Home-Page-Items/FY2018-IPPS-Final-Rule-Tables.html
- Shanafelt T, Goh J, Sinsky C (2017) The Business Case for Investing in Physician Well-being. JAMA Intern Med 177:1826-1832.
- Roberts DL, Shanafelt TD, Dyrbye LN, West CP (2014) Burnout and Work‐Life Balance. J Hosp Med 3:176-181.
- Vuong K (2017) Turnover Rate for Hospitalist Groups Trending Downward.
- Ericksen AB (2017) The Cost of Hiring Locum Tenens for Your Practice or Facility.
- Schutte L, Search C, Louis St (2012) Building a Business Case for Recruitment and Retention Best Practice.
- Locum Tenens (2018) Locum Tenens Vs. Permanent Physicians: Compare the Costs.
- Tiem JMV, Steffensmeier KRS, Wakefield BJ, Stewart GL, Zemblidge NA, et al. (2019) Taking note: A qualitative study of implementing a scribing practice in team-based primary care clinics. BMC Health Services Research 19.
- Huff H (2012) Scribes: A write way and a wrong way. ACP Internist.
- Bailey M (2016) The Pay Is Low, The Typing Nonstop, But The Medical Scribe Business Is Booming. STAT.
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences