Atypical Case of Lung Hernia which Looked like a Flail Chest after Trauma
Bassem Alhadia and Shammy Rashid Alib*
Department of Emergency Medicine, Mater Misericordiae University Hospital, Dublin, Ireland
- *Corresponding Author:
- Shammy Rashid Alib
Department of Emergency Medicine,
Mater Misericordiae University Hospital, Dublin,
Ireland,
E-mail: sshammy@hotmail.com
Received date: March 28, 2023, Manuscript No. IPJHMM-23-15601; Editor assigned date: March 31, 2023, PreQC No. IPJHMM-23-15601 (PQ); Reviewed date: April 14, 2023, QC No. IPJHMM-23-15601; Revised date: April 21, 2023, Manuscript No. IPJHMM-23-15601 (R); Published date: April 28, 2023, DOI: 10.36648/2471-9781.9.2.353
Citation: Alhadia B, Alib SR (2023) Atypical Case of Lung Hernia which Looked like a Flail Chest after Trauma. J Hosp Med Manage Vol.9 No.1: 353.
Abstract
Lung hernia, also known as pulmonary hernia or intercostal herniation is when the lung parenchyma protrudes beyond the normal limits of the thoracic wall. Pulmonary hernias are extremely rare and can be congenital or acquired. Most lung hernias are the result of injury or trauma to the chest area, such as a fall or car accident. We present a case of a seven-year-old child who developed a pulmonary hernia following a fall from his bike, slamming the bike handle onto the chest wall. We describe the clinical features, diagnosis, and successful treatment.
Keywords
Pulmonary hernias; Lung hernia; Trauma; Clinical features
Introduction
Pulmonary hernia is a protrusion of the lung beyond the normal limits of the thoracic cavity, because of a defect in the thoracic wall. Pulmonary hernias are extremely rare occurrences and are seen following a traumatic event or a surgical procedure. Pulmonary hernias were first described by Roland, in 1499. Currently, lung hernias can be classified according to location (i.e., cervical, thoracic, or diaphragmatic) and aetiology [1]. Most cases of lung hernia are acquired, usually related to trauma or surgery. Symptoms can vary and usually a painless, local, and inconstant bulging is evident on physical examination. The diagnosis of a lung herniation is accomplished using chest radiographs generally. Surgery is usually reserved for large hernias or incarcerated hernias [2].
Case Presentation
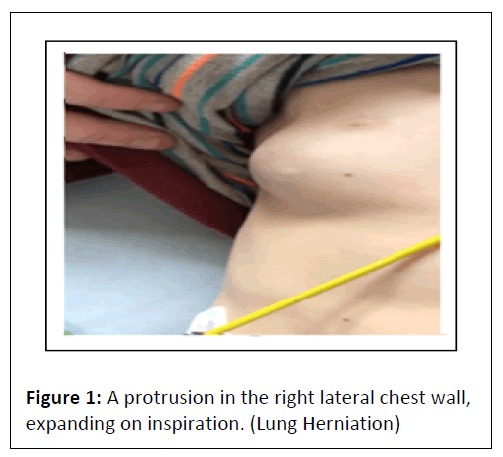
A seven-year-old male fell from his bike and suffered blunt chest trauma after striking his chest wall onto the handle of the bike. Physical examination of the right lateral chest wall revealed a mass with paradoxical motion during respiration. He had mild pain but denied breathing difficulty. His respiratory movements caused the swelling to vary and enlarge with Valsalva maneuvers. He was stable clinically as given by Figure 1.
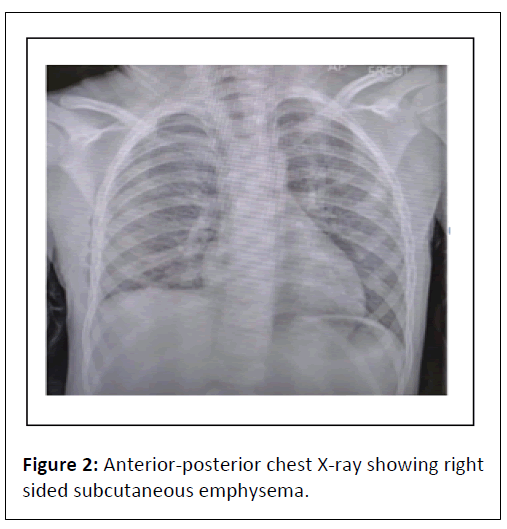
Radiographs of the chest demonstrated no ribs fracture, pneumothorax or lung contusion. The child held his breath during the X-ray so there was no evidence of the hernia in the film (Figure 2).
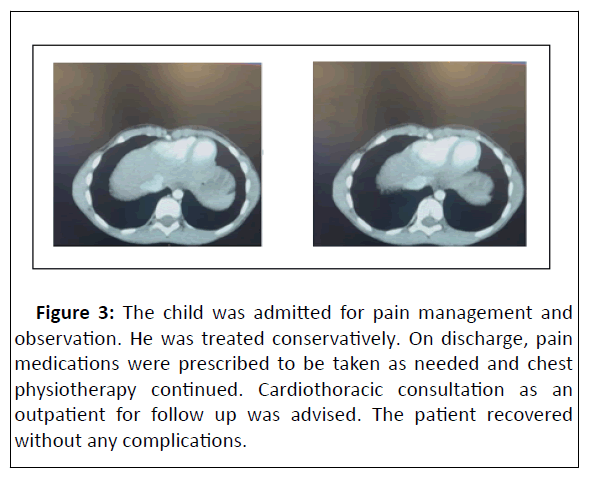
CT thorax and abdomen was done which revealed right pleurocutaneous fistula, pneumothorax, surgical emphysema and pneumomediastinum. No rib fractures or consolidation were seen in Figure 3.
Figure 3: The child was admitted for pain management and observation. He was treated conservatively. On discharge, pain medications were prescribed to be taken as needed and chest physiotherapy continued. Cardiothoracic consultation as an outpatient for follow up was advised. The patient recovered without any complications.
Discussion
Intercostal hernias or pulmonary hernias, refers to a part of a lung pushing through a tear, or bulging through a weak spot, in the chest wall, neck passageway or diaphragm. Pulmonary hernias can be classified as congenital or acquired. Congenital hernias are the result of a weakness in the thoracic wall or an increased intrathoracic pressure whereas acquired hernias could be classified as either traumatic or pathological hernias, wherein the weakening of the thoracic cage is caused by either injury or disease [3].
Acquired hernias are usually associated with some type of blunt trauma to the chest wall. Blunt trauma resulting in herniation of the lung is extremely rare in the pediatric population. These herniations are often associated with rib fractures [4]. The penetrating injury also results in herniations but is far less common as compared to blunt injuries [5]. Motor vehicle accidents are the most common cause of such herniations. Morel-Lavalle established a classification in 1845 according to the location and cause of the lung hernia. Most lung hernias are frequently acquired due to traumatic injury. Their position may be thoracic (65%), cervical (35%), or rarely transdiaphragmatic. In children, lung hernias are most often next to the sternum, in a context of a sternocostal dislocation [6].
It is important to recognize that the development of lung hernia requires a combination of anatomical and physiological factors. To promote migration of lung tissue outside its usual domain there must be weakness or defect in the structural boundaries and sudden or chronic increase in intrathoracic pressure. For cervical herniations, a defect in Sibson’s fascia is identified whereas for thoracic herniation there is separation or fracture of ribs with weakening of the intercostal muscles. The eventual herniation of lung through these weakened areas occurs when intrathoracic pressure increases as seen in chronic cough or significant chest impact.
Clinically, the symptoms can range and vary from relatively mild to unmistakably evident. Since this is so rare, the diagnosis is often missed. In case an intercostal mass is present; it could vary in size with respiration and show paradoxical protrusion during expiration. The intercostal mass will be reducible and elastic and may be associated with overlying crepitus. Imaging when done will show the most common finding on chest X-ray as a well-circumscribed loculation of subcutaneous air. CT can be done to better visualize the thoracic cage and pleural space and to rule out associated injuries [6]. A sagittal incidence chest Xray, with increased intra-thoracic pressure during radiography, can confirm the diagnosis in most cases. Another diagnostic option is ultrasonography. In trauma, patients are evaluated with the eFAST or extended focus assessment with sonography in trauma. This rapid diagnostic test involves assessment of the pleural cavities to identify pneumothoraces and can be of much use especially in the emergency department.
Treatment options include observation or surgical repair. Factors determining the treatment plan include the location of the hernia and the presence of symptoms. Large defects normally require repair with mesh. Supraclavicular herniations may be observed, while intercostal herniations require immediate repair. It has also been stated that asymptomatic cases may be observed, while those with severe symptoms e.g. haemoptysis, recurrent respiratory infections, or those threatening to strangulate, must be repaired [7].
Clinical monitoring is recommended in cases of small asymptomatic hernia, but if the hernia becomes larger with or without symptoms, surgical treatment is indicated. When a patient is diagnosed with LH, it is paramount that the etiology, location, and associated symptoms are assessed and evaluated to determine treatment [8]. Conservative treatment is the best option in most cases of asymptomatic small lung herniation, with low risk of strangulation as well as the risk of recurrence being low. In our case, our patient was treated conservatively.
Conclusions
• In our case, treatment was conservative which included pain control, observation and chest physiotherapy during and after admission then with outpatient cardiothoracic follow-up. The patient had an uneventful hospital course and was discharged stable.
• There is limited literature on pulmonary hernia, especially in the pediatric population. It is crucial to get prompt diagnosis and treatment as the entrapment of herniated lung may lead to ischemic complications of lung tissue. Due to its rarity, lung hernia management standards have not been established.
• Diagnostic thoracoscopy may be considered in any child who presents with a possibility of pulmonary herniation in order to further quantify the injury to the chest wall as well as other potential injuries within the thorax. Thoracoscopy is useful for the visualization of the intrathoracic wall and lung parenchyma and plays an excellent role in the repair of the hernia.
• Our patient currently has no symptoms after the healing of his intercostal muscles and has recovered quite well and has incurred no respiratory complications.
Conflicts of Interest
The authors declare that there is no conflict of interests regarding the publication of this paper.
References
- Moncada R, Vade A, Gimenez C, Rosado W, Demos TC, et al. (1996) Congenital and acquired lung hernias. J Thorac Imaging 11: 75-82.
[Crossref], [Google Scholar], [Indexed]
- Fitzpatrick C, Coppola CP, Eichelberger MR (2007) Intercostal hernia and spontaneous pneumothorax in a liver transplant recipient: A case report. J Pediatr Surg 42: E5-E8.
[Crossref], [Google Scholar], [Indexed]
- Sandrasagra FA, Di-Eusanio G, Hamilton DI (1979) Traumatic intercostal hernia due to a nonpenetrating injury in a child. J Pediatr Surg 14: 471-472.
[Crossref], [Google Scholar], [Indexed]
- Lum Min SA, Gow KW, Blair GK (1999) Traumatic intercostal hernia: Presentation and diagnostic workup. J Pediatr Surg 34: 1544-1545.
[Crossref], [Google Scholar], [Indexed]
- Allen GS, Fischer RP (1997) Traumatic lung herniation. Ann Thorac Surg 63: 1455-1456.
[Crossref], [Google Scholar], [Indexed]
- Francois B, Desachy A, Cornu E, Ostyn E, Nlquet L, et al. (1998) Traumatic pulmonary hernia: Surgical versus conservative management. J Trauma 44: 217-219.
[Crossref], [Google Scholar], [Indexed]
- Gomes TN, Pereira MC, Smith SC, Melgar TA (2022) Lung herniation associated with crack cocaine use: An uncommon cause of chest pain. Cureus 14: e21801.
[Crossref], [Google Scholar], [Indexed]
- Morel-Lavallee A (1847) Hernie du poumon. Bull Mem Soc Chir Paris: 75–95.
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences