Chemotherapy Induced Takotsubo Cardiomyopathy
Muhammad Bilal, Shammy Rashid Ali, Muhammad Usman Raza, Michael Molloy, Paul Kelly, Eoin Kelly, Muhammad Shahzad.
DOI10.36648/2471-9781.21.7.286
Muhammad Bilal*, Shammy Rashid Ali, Muhammad Usman Raza, Michael Molloy, Paul Kelly, Eoin Kelly, Muhammad Shahzad
Department of Emergency Medicine, Wexford General Hospital, IrelandDepartment of Emergency Medicine, Wexford General Hospital, Ireland
- *Corresponding Author:
- Muhammad Bilal
Department of Emergency Medicine, Wexford General Hospital, Ireland
Tel: 00353851080460
E-mail: bilal_dr87@yahoo.com
Received Date: July 21, 2021; Accepted Date: August 12, 2021; Published Date: August 19, 2021
Citation: Bilal M, Ali SR, Raza MU, Molloy M, Kelly P, et al. (2021) Chemotherapy Induced Takotsubo Cardiomyopathy. J Hosp Med Manage Vol.7 No.8:286.
Introduction
In the early 1990s, Japanese authors reported a reversible cardiomyopathy that seemed to be precipitated by acute emotional stress [1]. More than 90% of reported cases are in women suspected of having a heart attack actually have this disorder [2].
Takot subo Cardiomyopathy is characterized by transient ventricular systolic dysfunction in absence of obstructive coronary artery disease, typically accompanied by ST-Segment changes / T wave inversions with raised Troponin levels. TC (stress induced cardiomyopathy, broken heart syndrome), so named due to appearance of left ventricles resembling “Japanese octopus pot”.
Chemotherapeutic agents have been linked to TC including 5-fluorouracil (5 FU), capecitabine, cisplatin/docetaxel, cytarabine, cytarabine/daunorubicin [3]. The pathogenesis of chemotherapy-induced TC remains uncertain but is mostly attributed to the emotional and physiological stress related to underlying malignancy, direct cardio toxicity caused by the free radicals and possible para neoplastic phenomenon [4].
Fluorouracil is the most commonly reported TS-triggering chemotherapeutic agent, although this must be interpreted in the context of the frequency of worldwide use of this agent [5].
Case Representation
A 57 years old female presented to ED with multiple episodes of central chest pain radiating to left arm and a pre-syncopal episode. She had 1st cycle of chemotherapy (Folfox-5-Flurouracil) 2 days ago for colonic adenocarcinoma. Asymptomatic on arrival. Initial bloods, ECG, Troponin and chest X-Ray were normal (Figure 1).
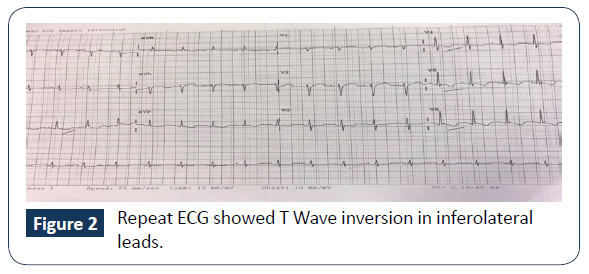
She had another presyncopal episode, became pale, diaphoretic and hypotensive 90/60. Repeat ECG showed T Wave inversion in infer lateral leads. Both Troponin (0.31), D-Dimer (7.34) were elevated (Figure 2).
Management and Outcome
Patient was given a bolus of fluid challenge for which she did not respond and had persistent hypotension had another pre syncopal episode and was still hypotensive with maximum BP 61/37.
As the BP further dropped to 39/28 HR 70 beats/minutes a bolus of phenylephrine and metaraminol given. Dobutamine infusion started with good effect. ACS protocol initiated and in view of PE
She was admitted in Critical care.
POCUS demonstrated RV hyperkinesia, LV dilated with severe global dysfunction, dilated IVC and LVEF 15%. Profound hypotension requiring dobutamine infusion and subsequent admission to CCU. Departmental echocardiogram confirmed the initial findings (Figure 3),
CT Pulmonary angiogram was negative for P.E.
Coronary angiogram revealed non-obstructing coronary arteries and normal ventricular systolic functions with final diagnosis of Takotsubo Cardiomyopathy. She was discharged on LMVH and Ramipril. Follow up Echocardiogram after 5 weeks, demonstrates normal LV function with EF 50-60%.
Patient reviewed by Oncology and changed chemotherapy to camptothecin-11.
Discussion
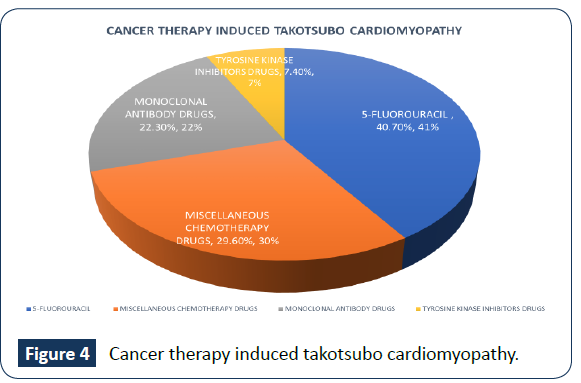
TC is reversible cardiomyopathy associated with physical/ emotional stresses. It is rare complication of chemotherapy, Only 27 cases of cancer related therapies have been reported since 2000. , 19 of those attributed to chemotherapy, 6 to monoclonal antibodies, 2 to tyrosine kinase inhibitor, 11 (40.7%) has had 5-FU as part of chemotherapy regimen, 8 were poly-chemotherapies. 5-FU is the most common drug associated to Takotsubo cardiomyopathy. Cardiotoxicity is a known adverse effect of FU and occurs in 1.2% to 18% of patients who receive the agent [6]. Probable mechanism is 5-FU mediated formation of circulating micro thrombi due to kallikrein micro thrombi generation leading to ventricular dysfunction [7] (Figure 4).
References
- Bybee KA, Prasad A (2008) Stress-related cardiomyopathy syndromes. Circulation 118: 397-409.
- Prasad A (2008) American Heart Journal. Am J Med Genet Suppl 155: 408-17.
- Smith SA, Auseon AJ (2013) Chemotherapy-induced takotsubo cardiomyopathy. Heart Failure Clin 9: 233-242.
- Inayat F, Masab M, Gupta S, Ullah W (2018) New drugs and new toxicities: pembrolizumab-induced myocarditis. BMJ Case Rep 223- 252.
- Goldberg N, Chaudhry H, Ackery A, Sholzberg M (2017) Reduced Reducing Unnecessary Coagulation Testing in the Emergency Department. BMJ Qual Improv Rep 130: 55-81.
- Ozturk MA, Ozveren O, Cinar V, Erdik B, Oyan B (2013) Takotsubo syndrome: an underdiagnosed complication of 5-fluorouracil mimicking acute myocardial infarction. Blood Coagul Fibrinolysis 24:90-94.
- Becker K, Erckenbrecht JF, Häussinger D (1999) Cardiotoxicity of the antiproliferative compound fluorouracil Drugs.Europe pmc 57: 475- 484.
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences