Comparison and Analysis of Health Care Delivery Systems: Pakistan versus Bangladesh
Santosh Kumar and Suria Bano
DOI10.4172/2471-9781.100020
Santosh Kumar* and Suria Bano
Aga Khan University School of Nursing and Midwifery, Karachi, Pakistan
- *Corresponding Author:
- Kumar S
Aga Khan University School of Nursing and Midwifery
Karachi, Pakistan
Tel: +92 333-3267825
E-mail: santoshkumarpak@gmail.com
Received date: December 22, 2016; Accepted date: January 09, 2017; Published date: January 14, 2017
Citation: Kumar S, Bano S. Comparison and Analysis of Health Care Delivery Systems: Pakistan versus Bangladesh. J Hosp Med Manage. 2017, 3:1.
Abstract
Health Care Delivery System (HCDS) is the arrangement that serves best to any country’s population with effective, efficient, fair distributions of resources, and funds for organized infrastructure to thrive well. Globally, HCDS becomes a highly competitive and rapidly growing service and needs special attentions from different domains. The optimal HCDS provides hope, relief to the individual, community, and population. The balanced health care system delivers the quality of care, health, and facilities through efficient, effective, and fair manner. Moreover, across the world the HCDS varies from country to country and focusing on improving access, coverage and quality of services, however, it depends on the key resources being available, organized, managed, and utilized effectively. In this paper, we will discuss HCDS of Pakistan in comparison to Bangladesh with areas of governance, service delivery, finance, information, human resources, and medical technologies and will analyze HCDS of both countries, and ends with challenges, recommendations to improve health care reforms and its utilization.
Keywords
Pakistan; Bangladesh; Health care delivery system; Health indicators; Health issues
Introduction
Health Care Delivery System (HCDS) is a societal response to the determinants of health. The concept of health care system includes the involvement of the people, organizations, agencies, and resources that provide services to meet the health needs of the individual, community, and population [1]. The fundamental premise of the HCDS is to value human life, promote, restore, and maintain the health of the population and that is focused and organized around the health needs and expectations of people [2]. The effectiveness of health care system depends upon human, materials, finance, availability and accessibility of resources. The optimal HCDS integrates the different health services encompasses the management and delivery of quality and safe health services [3]. Moreover, in the balanced health care system people receive a continuum of health promotion, disease prevention, diagnosis, treatment, disease management, rehabilitation and palliative care services, through the different levels and sites of care within the health system, and according to their needs throughout the life course [4]. Now, in this paper, we will discuss, compare, and analyze the HCDS of Pakistan in comparison to Bangladesh.
Demographics of Pakistan and Bangladesh
Pakistan is a located in South Asia encircled by Afghanistan, India, China, Arabian Sea and Iran. It is the 36th largest country in the world in terms of area with an area covering 881,913 km2 (340,509 sq mi). Pakistan is the sixth most populous country in the world, with about 185 million people and by 2050 it will become the fourth largest populated country in the world [5]. The United Nations Development Programme (UNDP) ranked Pakistan in the Human Development Index (HDI) 146th out of 187 countries. Presently, Pakistan has Gross Domestic Product (GDP) stagnant at 4.71%, Gross National Income (GNI) per capita is approximate US$ 1550, and is categorized as low-income country and positioned at 65th among 102 developing countries. Currently, the literacy rate of the population has increased to 58% as compared to 53% in 2011-12 [6]. The state religion in Pakistan is Islam, practiced by 95-97% of the population, and remaining 3-5% practice Christianity, Hinduism, and other religions. Bangladesh is one of the most densely populated South Asian countries. It occupies 147, 570 square kilometers. It is the ninth most populated country in the world, in 2013 had a population of 156.6 million that is expected to increase to around 218 million by 2030 [7]. Recently, Bangladesh has undergone considerable social and economic changes, economy dramatically accelerated and GNI increased from US$ 100 per capita in 1973 to US$ 700 in 2010 [8]. The country is experiencing a high rate of urbanization despite such rapid urbanization, Bangladesh is still primarily a rural country with more than seventy percent of the population living in rural areas [9]. The UNDP ranked Bangladesh as 146th out of 187 countries in terms of HDI. Islam is the faith of eighty-five percent of the population, while Hindus, Buddhist, and Christians making up the most of remaining fifteen percent.
Pakistan Health Care Delivery System
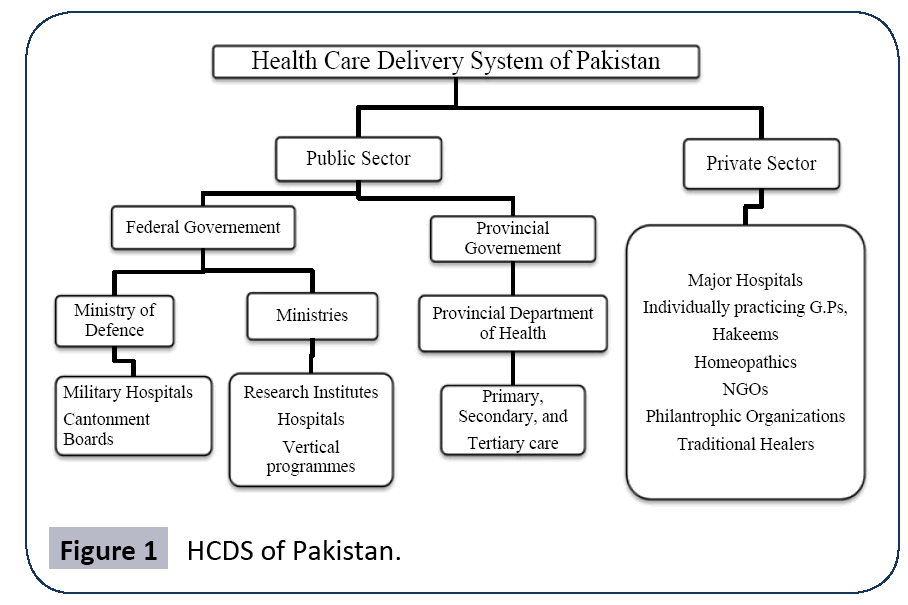
Pakistan has a mixed health system that includes public, parastatal, private, civil society, philanthropic contributors, and donor agencies. In Pakistan, health care delivery to the consumers is systematized through four modes of preventive, promotive, curative, and rehabilitative services. The private sector attends 70% of the population through a diverse group of trained health team members to traditional faith healers [10]. Both vertical and horizontal HCDS exists in Pakistan. The HCDS of Pakistan is summarized in Figure 1. The major strength of HCDS of Pakistan is an outreach primary health care services delivered at the community level by Lady Health Workers (LHWs), Lady Health Visitors (LHVs), and Community Midwives (CMWs) who have earned success and trust in the communities [11]. In Pakistan, these LHVs, LHWs, and CMWs are attached to the government facilities, from which they receive training, and serve the community at the doorstep in order to get desired health outcomes. Furthermore, in Pakistan under article 18th amendment the health care services are the obligations of provisional government except for the federal area. The public health delivery system functions through a three layer approach primary, secondary, and tertiary (Figure 1).
Bangladesh Health Care Delivery System
Over the 45 years after independence, the HCDS of Bangladesh has gone through a number of reforms and established an extensive health infrastructure [12]. The provision of basic health services in Bangladesh is pluralistic with four key actors that define its structure and function: government, private, non-governmental organizations (NGOs), and donor agencies [13]. In the early phase, the health system of Bangladesh was primarily focused on providing curative services but at present with the involvement of United Nations, private sectors, NGOs, and donor agencies the health system has shifted its emphasis equally both on curative and preventive services [14]. Though, HCDS has expanded its reach despite the people of rural areas remains with little access to facilities [8]. Moreover, the HCDS of Bangladesh is challenged with governance, finances, human resources, service delivery, technology, manpower, and essential supplies like medicines [15].
Key Health Issue and Indicators
In Pakistan since 2000, there has been the notable improvement in some health indicators mainly as a result of public, private programs and NGOs contributions [16]. Despite, health profile of Pakistan is illustrated by high population growth rate, infant and maternal mortality rates, and dual burden of communicable and non-communicable diseases [17]. Regardless, the country is undergoing considerable social, environmental, and economic changes. The basic food requirement and health are problems for the people, the paper by Nishtar [18] indicated that malnutrition is worst in the rural areas of Sindh, and Baluchistan with 20-30% children are being retarded, and high infant mortality is as a result of malnutrition, diarrhea, and pneumonia. Furthermore, about 40% of deliveries are attended by skilled birth attendants, and the high maternal mortality rate is related to high fertility rate, low skilled birth attendance, malnutrition and inadequate access to emergency obstetric care services [19]. The key demographic and health indicators of both countries are summarized in Table 1. Bangladesh despite its challenging circumstances, has proven to be remarkably resilient and achieved significant human development gains, and impressive progress was made in health outcomes, especially in maternal and child health [20]. Population growth slowed considerably during the past thirty years and falling from 2.7 percent per year in the 1980s to around 1.3 percent in 2010 [21]. The contributions of the overall disease in terms of percentages in Pakistan and Bangladesh are shown in Table 2.
| Indicators | Pakistan | Bangladesh |
|---|---|---|
| Population under 15 years | 34% | 30% |
| Population over 60 years | 7% | 7% |
| Infant mortality rate/1000 | 42 | 41 |
| Maternal mortality rate/100,000 | 170 | 170 |
| Crude birth rate/1000 | 31 | 20 |
| Crude death rate/1000 | 8 | 5.59 |
| Fertility Rate (F.R) | 3.2 | 2.2 |
| Immunization coverage | 65% | 87.5% |
Table 1: Key Demographic and Health Indicators.
| Diseases | Pakistan | Bangladesh |
|---|---|---|
| Communicable, maternal, perinatal, and nutritional diseases | 41% | 46% |
| Non-communicable diseases | 59% | 54% |
| CVDs | 21% | 23% |
| Injuries | 16% | 10% |
| Cancer | 6% | 7% |
| Diabetes | 2% | 1% |
| Respiratory diseases | 7% | 5% |
| Other Chronic diseases | 7% | 8% |
Table 2: Contributions of the disease.
Goals and Expectation
Since the time of independence, HCDS of Pakistan has undergone major reforms start its journey from National Health Policy, Primary Health Care services, TB control, and Immunization Program [22]. Regardless of settled goal and expectations Pakistan health system showed dissatisfactory progress and failed to achieve desired outcomes [23]. Furthermore, Pakistan failed to achieve goals of “Health for All” in Alma Ata Declaration and failed to attain Millennium Developmental Goals (MDGs) 2015. Currently, Pakistan is aiming to attain the Sustainable Development Goals 2025. In addition, Pakistan has also settled the National Health Vision 2016-25 to improve the health of all population particularly women and children, through universal access to affordable quality essential health services, and delivered through resilient and responsive health system. On the other hand, Bangladesh has surpassed many neighboring countries in South Asia as well as other developing countries in terms of progress in achieving the health-related MDGs. Similarly, Bangladesh also achieved significant progress towards achieving the twin goals of eradicating poverty and promoting shared prosperity 2007. Furthermore, Bangladesh became successful in achieving almost universal immunization coverage and reducing child and maternal deaths. Recently, Bangladesh has set National Five Year Strategic Investment Plan (SIP) in order to improve the health of the population, reforming the institutions, and improving performance. However, poor access to services, low quality of care, and high rate of mortality and poor status of child health still remain as challenges of the health sector of Bangladesh [24].
Comparison and Analysis of health care system of Pakistan and Bangladesh
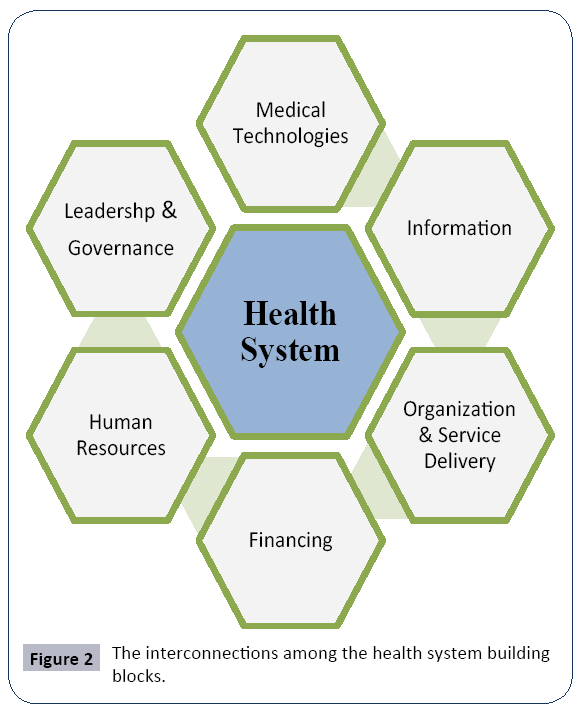
Health systems encompass not only various elements but also the interactions and relationships between those elements and individuals within the system [25]. The de Savigny & Adam developed a framework that shows relationaship and interactions among the different domain of the health care delivery system (Figure 2).
Leadership and Governance
The Pakistan HCDS is mixed, referring to the existence of multiple actors performing diverse roles and functions. Currently, health services in Pakistan are a major obligation and constitutionally a provincial subject except for federally administered areas. The health care delivery has traditionally been jointly administered by the federal and provincial governments with districts mainly responsible for implementation. Presently, the Ministry of National Regulations and Services plays a key role in the formulation of policies, strategies, setting a vision, and planning. The operationalization of the policies and laws lies on the provisional and local governments. Whereas, in the HCDS of the Bangladesh the Ministry of Health and Family Welfare (MOHFW) is the authoritative body, and little authority delegated to local levels as the comparison to the Pakistan. The MOHFW is not only responsible for setting entire policies and regulations but also for providing comprehensive health services, financing and health staff. The MOHFW has Directorates of General and Health Services (DGHS) and Family Planning (DGFP) that manage the dual system of general health and family planning across the country. In addition, the Ministry of Local Government, Rural Development, and Cooperatives play their part and manage the provision of urban primary care services.
Health System Organizations and Service Delivery
Organization is the system of consciously coordinated activities, goal-directed efforts for the controlled performance of collective goals [26]. The health system of Pakistan has different tiers of organizations and delivery service. In Pakistan, the Primary health care facilities are provided by Government Dispensaries (GD), Basic Health Units (BHU) at the village level, and Rural Health Centers (RHC) at the level of the town. Secondary health care facilities include Taluka Head Quarters (THQs), and District Head Quarter (DHQs) at the level of taluka, district and large cities respectively. In addition, Maternity and Child Health Centers (MCHCs) play their part and provide basic obstetric care the community with the collaboration of lady health workers. The statistics of the health care facilities in Pakistan is shown in Table 3. The health care service delivery in Bangladesh starts from the Community Clinics (CC) in villages, Union Health and Family Welfare Centers (UHFWC) at unions (collection of villages), Upazila Health Complexes (UHC) at the sub-district level, and backed by District Hospital (DH). The core primary health care facilities in Bangladesh are CCs. The DHs, UHCs, and UHFWC contributing their part in secondary and tertiary care with more advanced facilities. Bangladesh health care services are shown in Table 3. Both the Pakistan and Bangladesh seeks to create conditions whereby the people have to access and attain the highest level of health.
| Types of Hospital in Pakistan | Numbers of Hospitals | Types of Hospital In Bangladesh | Numbers of Hospitals |
|---|---|---|---|
| Public Hospital | 924 | District Hospital | 53 |
| Dispensaries | 4,916 | General Hospital | 11 |
| Basic Health Units | 5336 | Infectious Disease Hospital | 180 |
| Rural Health Centers | 595 | Chest Disease/TB Hospital | 13 |
| MCH Centers | 1,138 | Leprosy Hospital | 03 |
| TB Centers | 371 | Specialized Centers | 03 |
| First Aid Points | 1080 | Upazila Health Complex | 425 |
| Population per bed | 1,515 | Union Health and Family Welfare Centers | 1469 |
| Population to health facility ratio | 11,413 | Community Clinics | 12,248 |
Table 3: Health care services in Pakistan and Bangladesh.
Health Financing
Currently, Pakistan is spending 0.4% of its GDPs on health and this amount is about 50 billion PKR . The funding is dominated by out of pocket payments, government revenues, developmental partners, private insurances, external resources to NGOs and world funding [27]. Out-of-pocket expenses refer to costs that individual, organization, or state pay out of their own cash reserves. It is direct outlays of cash that may be later reimbursed [28]. Though, no official figure exists for health expenditures and expert believes that 78.08% is contributed through the outof- pocket mechanism, general taxation is the major source of government’s financing for health [29]. Previously, provincial governments were responsible for health financing but currently as a result of political and administrative devolution empower district governments as important financial intermediaries. About 60% of the total government health expenditure is therefore accounted for in district budgets. Several organizations and donor agencies have made significant contributions to improve health outcomes in Pakistan for over last few decades. The foreign aid as a percentage of total health sector allocation is about 2% only. The main internal NGOs and agencies contributing in the health system are HANDS, Shiffa Foundation, and Aga Khan Health Services Pakistan (AKHSP). In addition to the internal resources, the external funding agencies in Pakistan are USAID, and Department for International Development, UK. Currently, National Tuberculosis Control Program, EPI programs, diagnostic kits for the HIV/AIDS program, and Hepatitis program is governed by donor agencies at Pakistan.
As per the report of Bangladesh National Health Accounts (NHA), Bangladesh spends US$ 2.3 billion on health yearly, and approximately 64% of the amount comes from out-of-pocket payments. The public funds for health are the main prepayment mechanism for risk-pooling and constitute 26% of total health expenditure. Currently, Bangladesh spends US$ 26.60 per capita in total [17]. The Bangladesh government health expenditures as a share of GDP grew to 4.7% in 2015 which was around 1% till 2007. Moreover, the financing for health expenditures in Bangladesh comes from the different sources via different mechanism and payments. The world funds and external resources to NGOs has been also an important source of health financing in Bangladesh.
Bangladesh gets 8% of total health expenditures from donor agencies since 2007. In addition to internal resources, the main external funding agencies in Bangladesh are Global Alliance for Vaccines and Immunization (GAVI), Global Fund to Fight AIDS, Tuberculosis and Malaria (GFATM), and USAID. However, some donors pool their fund and channel that through government system while other donors directly through project not channeling the government system [30].
Human Resources
Pakistan is the sixth most populated country in the world, and as per the requirement of the population, the health human resources are insufficient. Pakistan is listed as one of 57 countries with critical health workforce deficiency [31]. Today, doctor to patient ratio in Pakistan 1:1300, doctor nurse ratio is 1:2.7, and nurse-patient ratio is 1:20 (Nishtar, 2006). The WHO suggests that doctor to patient ratio should be 1:1000 and doctor nurse ratio 1:4 is appropriate. Moreover, Pakistan Nursing Council recommends that nurse-patient ratio in general area is 1:10, and in specialized are is 2:1. Likewise, the most critical challenge faced by the health systems in Bangladesh is also in the arena of human resources. Moreover, Bangladesh has one of the worst nursephysician ratios, and it has only one nurse per three physicians. Furthermore, absenteeism, inefficiency, and corruption are also seen common in health setup of Bangladesh [8]. In the health care arena of Bangladesh, the doctor to patient ratio is 0.58:1000, and nurse-patient ratio is 0.3:1000 (Bangladesh Health Watch 2008; WHO, 2009). The statistics of health professionals at Pakistan and Bangladesh is shown in Table 4. There is a large cadre of health care providers in the informal sector is evident in both Pakistan and Bangladesh. It comprised of unqualified allopathic providers (e.g., rural doctors, drug shop retailer), traditional healer, faith healer, Unani, and semi qualified allopathic providers (e.g., medical assistants, technician, and community health worker). Though these are not part of mainstream health system but a major health care provider to poor rural population, especially in remote and hard to reach an area.
| Types of Health Care Provider | Pakistan | Bangladesh |
|---|---|---|
| Doctors | 139,555 | 91,000 |
| Dentists | 9,822 | - |
| Nurses | 69,313 | 15 415 |
| Midwives | 26,225 | 16,559 |
| Medical Technologists | 7,891 | 9,249 |
| Health Visitors | 10,731 | 5,411 |
| Registered Vets | 4800 | - |
Table 4: Health professionals statistics.
Medical Products
The health system of Pakistan expands more than eighty percent of their health expenditures on medical products and pharmaceuticals [32]. It has no pharmaceuticals industry at a time of independence. Currently, a pharmaceutical industry of Pakistan is rapidly developing and has 411 registered manufacturing divisions and 30 multinational companies across the country. It meets approximately 80% of country’s demand and 20% are being imported [10]. The Drug Regulatory Authority of Pakistan (DRAP) is the authority that set policies, rules, and control pharmaceutical companies. In 2010, the authority has been shifted to provincial government from federal, and it has four directional boards. The primary objective of the authority is to ensure the quality, effectiveness, drug safety, implementing the policies and guidelines. Moreover, it confirms the performance, laws enforcement, and ensure the safe medication manufacturing. Drug prices in Pakistan are controlled under the section 12 of Drug Act 1976 which gave the authority to Ministry of National Regulation and Services to control over the pricing of drugs. However, in Bangladesh, the Directorate General of Drug Administration (DGDA) is the supreme regulatory authority for drug-related affairs such as licensing, production, import, export, quality control and pricing [33]. The DGDA is a regulated by Director General and assisted by four directors responsible for manufacturing, licensing, quality control and drug testing. Bangladesh has two drug testing laboratories one in Chittagong, other in Dhaka. Bangladesh has National Drug Policy Act 1982 whose prime objective is to provide the quality essential drug at an affordable price. From 1981 to 1991 the price of drugs was increased only 20% in local currency. Thereafter, from 1992 to 2009 price was increased by 15%. Since 2010, the leading pharmaceutical companies have significantly increased the prices of drugs up to 8-10% including some common drugs on basis of raw material import become costlier [34].
Information, Research, and Technology
Pakistan health system has an extensive infrastructure spanning the country but has inadequate resource i.e. drugs, instruments, supplies, and technologies [11]. Health systems rely a great deal on health technologies; the limited use of information technology, record maintenance, and unfitting infrastructure can be observed in the health system of Pakistan [35]. It lacks Health Management Information System (HMIS) in public sector and has no well-defined policy and plans for technology implementation, telemedicine, and infrastructure development. Moreover, most of the health care educational institutions have limited tools and technology to prepare the health professionals. The process of certifying, licensing is weak and evaluation of the performance of health professional is not maintained across the country. At the national level the legislative framework for health information that covers vital registration and notifiable diseases reporting do not exist. However, certain private organizations in the country are well equipped with advanced technology, infrastructure, and HMIS. In addition, an armed force hospital across the country has well-built infrastructure, HMIS, and proper technology utilization. Moreover, the concept of e-health has been implemented in the rural areas of Pakistan e.g. Gilgit-Baltistan with the help of COMSATs university, and Association of Pakistani Physicians of North America [3]. Similarly, Bangladesh as compared to other developing countries is poor in the field of infrastructure, and human resources, and has no specific written policy for infrastructure development in the health sector [36]. However, during 2007-2013, a steady increase in the number of hospitals and beds is evident in both the public and private sectors. The public health sector facilities in Bangladesh are poorly equipped with medical equipment and instruments. In addition, Bangladesh has four different HMIS under the supervision of directorates but there is a poor linkage between them but all provide summarized data to the MHFW [37].
Challenges faced by Pakistan and Bangladesh Health Care System
The HCDS of both the countries is facing multiple challenges in services delivery to the population. Though in Pakistan, the infrastructure of health care centers like BHUs and RHCs are present but it is poorly maintained, not well equipped and lacks human workforce especially in rural areas. Simultaneously, the most critical challenge faced by the health systems in Bangladesh is in the arena of human resources, technology, and infrastructure [38]. The allocation of health care resources like finance and transport are not in use of need-based in the both countries. Moreover, due to high population in Pakistan and Bangladesh, the health care professionals are less according to the population of the countries and also the existing professionals are untrained, underpaid, and depressed of important facilities for their practice. To deal with the referrals to tertiary hospital, there is no transport facility to access emergency health care is found in the Pakistan. However, Bangladesh has a limited resources for transportation. The literature evident that in Pakistan and Bangladesh there is an inadequate opportunity for the health professional in the field of research and no advance technology was introduced in public sector of both countries. HCDS of both countries hugely relies on private organizations and these organizations provide the more advanced facilities but the whole population of the countries cannot afford these facilities. In Pakistan and Bangladesh, there are massive inequalities in the accessibility of health services to the low socioeconomic population. The majority of this population lives in the absolute poverty; they have to access public sector facilities, which are not providing satisfactory care [39].
Recommendations
The authors recommend that in order to improve the HCDS of Pakistan and Bangladesh several needs to be implemented.
The ministry and government should carefully allocate the available resources among the rural and urban population. The Government of both the countries should take initiatives in the development of human resources like doctors, nurses, and welltrained lady health workers. The stakeholders and the Ministry participate in the process of planning to implementation of healthcare program to maintain the sustainability of the program [40]. The health care providers to be trained in the use of modern technology, and policies to develop for E-health, HMIS, and promote development in the profession. Budget to be increased so they can become able to provide effective and efficient health to its population and achieve goals and expectations. The Government creates conditions whereby the people have the opportunity to reach and maintain the highest attainable level of health. Above all Pakistan and Bangladesh should immediately translate its health policies into action to benefit the people of the countries by ensuring humanity, equity, accessibility, and disease alleviation [41].
Conclusion
In the light of the findings of this paper, it can be fairly argued that both Bangladesh and Pakistan faces a lot of challenges in its health system. These challenges must be resolved in order to improve the existing health system so that the disadvantaged and vulnerable people can get better access to basic health care services. The paper emphasizes the importance of a multi-sectorial comprehensive approach to improve the health system. Moreover, Health cannot be separated from political, economic, social and human development contexts. The health system of Bangladesh and Pakistan desperately needs a dynamic leadership, governance that is prepared to design and enforce evidence-based policies and programs and taking care of the system. Furthermore, the steward of the health system must have a strategic vision and determination to improve and strengthen both the public and private health sectors of the country. In addition, equity must be the overarching guiding principle underpinning the health systems.
Acknowledgment
We would like to express our sincere gratitude Dr. Tazeen Saeed Ali, Associate Professor at Aga Khan University - School of Nursing and Midwifery Karachi and Dr. Aftab Mukhi for their continued support, motivations, and guidance at all the time.
References
- Mills A (2014) Health care systems in low-and middle-income countries. New England Journal of Medicine 370: 552-557.
- Starfield B, Shi L, Macinko J (2005) Contribution of primary care to health systems and health. Milbank quarterly 83: 457-502.
- Nishtar S (2006) The Gateway Paper: Health Systems in Pakistan, a Way Forward. Pakistan's Health Policy Forum.
- Hirshon JM, Risko N, Calvello EJ, Ramirez SSD, Narayan M, et al. (2013) Health systems and services: the role of acute care. Bulletin of the World Health Organization 91: 386-388.
- National Institute of Population Studies and ICF International (2013) Pakistan Demographic and Health Survey 2012-13. National Institute of Population Studies, Islamabad, Pakistan.
- https://data.worldbank.org/products/wdi
- https://apps.who.int/medicinedocs/documents/s17305e/s17305e.pdf
- Ahmed SM, Hossain MA, Chowdhury AMR, Bhuiya AU (2011) The health workforce crisis in Bangladesh: shortage, inappropriate skill-mix and inequitable distribution. Human Resources for Health 9: 3-10.
- Zaman HAKM, Alam KT, Islam JI (2010) Urbanization in Bangladesh: Present status and policy implications. ASA University Review 4: 1-16.
- Federal Bureau of Statistics, Government of Pakistan. National Education Census, 2014. Islamabad, Pakistan: Government of Pakistan, 2014.
- Ghaffar A, Kazi BM, Salman MD (2000) Health care systems in transition III. Pakistan, part I. An overview of the health care system in Pakistan. Journal of public health medicine 22: 38-42.
- Ahmed SM, Tomson G, Petzold M, Kabir ZN (2005) Socioeconomic status overrides age and gender in determining health-seeking behaviour in rural Bangladesh. Bulletin of the World Health Organization 83: 109-117.
- Mahmood SAI (2012) Health systems in Bangladesh. Health Res Policy Syst 1: 1.
- Aldana JM, Piechulek H, Al-Sabir A (2001) Client satisfaction and quality of health care in rural Bangladesh. Bulletin of the World Health Organization 79: 512-517.
- El Arifeen S, Christou A, Reichenbach L, Osman FA, Azad K, et al. (2013) Community-based approaches and partnerships: innovations in health-service delivery in Bangladesh. The Lancet 382: 2012-2026.
- https://www.who.int/whr/2000/en/
- Meghani ST, Sehar S, Punjani NS (2014) Comparison and Analysis of Health Care Delivery System: Pakistan versus China. International Journal of Endorsing Health Science Research 2: 46-50.
- Nishtar S, Boerma T, Amjad S, Alam AY, Khalid F, et al. (2013) Pakistan's health system: performance and prospects after the 18th Constitutional Amendment. The Lancet 381: 2193-2206.
- Collins CD, Omar M, Tarin E (2002) Decentralization, health care and policy process in the Punjab, Pakistan in the 1990s. Int J Health Plann Manage 17: 123-146.
- Chowdhury AMR, Bhuiya A, Chowdhury ME, Rasheed S, Hussain Z, et al. (2013) The Bangladesh paradox: exceptional health achievement despite economic poverty. The Lancet 382: 1734-1745.
- Farid KS, Ahmed JU, Sarma PK, Begum S (2011) Population dynamics in Bangladesh: data sources, current facts and past trends. Journal of the Bangladesh Agricultural University 9: 121-130.
- Shaikh B, Rabbani F, Safi N, Dawar Z (2010) Contracting of primary health care services in Pakistan: is up-scaling a pragmatic thinking. J Pak Med Assoc 60: 387-389.
- Shaikh BT, Mobeen N, Azam SI, Rabbani F (2008) Using SERVQUAL for assessing and improving patient satisfaction at a rural health facility in Pakistan. East Mediterr Health J 14: 447-456.
- Osman FA (2008) Health policy, programmes and system in Bangladesh achievements and challenges. South Asian Survey 15: 263-288.
- Frenk J (1994) Dimensions of health system reform. Health Policy 27: 19-34.
- Scott WR (2001) Institutions and organizations Ideas, Interests, and Identities. Sage Publications Inc.
- Ather F, Sherin A (2014) Health System Financing in Pakistan: Reviewing Resources and opportunities. Khyber Medical University Journal 6: 53-55.
- Russell L, Doggett J (2015) Tackling Out-of-Pocket Health Care Costs. University of Sydney, Australia.
- Islam A (2009) Bangladesh health system in transition: selected articles. 2009: James P. Grant School of Public Health, BRAC University.
- Islam A, Ahsan GU, Biswas T (2015) Health System Financing in Bangladesh: A Situation Analysis. American Journal of Economics, Finance and Management 1: 494-502.
- Rana SA, Sarfraz M, Kamran I, Jadoon H (2016) Preferences of doctors for working in rural islamabad capital territory, pakistan: a qualitative study. Journal of Ayub Medical College Abbottabad 28: 591-596.
- Azhar S, Hassali MA, Ibrahim MIM, Ahmad M, Masood I, et al. (2009) The role of pharmacists in developing countries: the current scenario in Pakistan. Human Resources for Health 7: 54-60.
- Chowdhury FR, Chowdhury MA, Chowdhury S (2005) Quality, Safety and Efficacy of drug in Bangladesh: Where we are. Journal of Medicine 6: 55-58.
- Financial System Management Unit (2015) Bangladesh economic review. Dhaka: Finance Division, Ministry of Finance.
- Punjani NS, Shams S, Bhanji SM (2014) Analysis of health care delivery systems: pakistan versus united states. Int J Endorsing Health Sci Res 2: 38-41.
- Ashad-uz-Zaman ASM, Rahman MDM, Shamsur Rahman M (2005) Poor People’s Access to Health Services in Bangladesh: Focusing on the Issues of Inequality. Network of Asia-Pacific Schools and Institutes of Public Administration and Governance (NAPSIPAG) Annual Conference 2005, Beijing.
- Bangladesh Health Watch (2007) Health Workforce in Bangladesh: Who Constitutes the Healthcare System? James P grant School of Public health, BRAC University, Bangladesh.
- Book SY (2015) Bangladesh Bureau of Statistics. Bangladesh Bureau of Statistics Dhaka, Bangladesh.
- Hall JJ, Taylor R (2003) Health for all beyond 2000: the demise of the Alma-Ata Declaration and primary health care in developing countries. Med J Aust 178: 17-20.
- Shaikh BT, Hatcher J (2005) Health seeking behaviour and health service utilization in Pakistan: challenging the policy makers. Journal of public health 27: 49-54.
- https://databank.worldbank.org/data/download/WDI-2013-ebook.pdf
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences