Digoxin: Decline in Prescribing
Muhammad Shahzad, Amir Taj Khan, Zulfiqar Sandhu, Salman Ashraf, Mian Shariq and Zaid Almadani
DOI10.36648/2471-9781.21.7.296
Muhammad Shahzad1*, Amir Taj Khan4, Zulfiqar Sandhu3, Salman Ashraf2, Mian Shariq2 and Zaid Almadani2
1St Vincent University Healthcare Group, Elm Park, Dublin 4, Ireland
2Causeway Hospital, Northern Ireland Health and Social Care Trust
3Wexford General Hospital, Wexford Ireland
4District Hospital Daggar, Buner, KPK
- *Corresponding Author:
- Muhammad Shahzad
St Vincent University Healthcare Group, Elm Park, Dublin 4, Ireland
Tel: 019198438075
E-mail: nimih70@icloud.com
Received Date: October 06, 2021; Accepted Date: October 22, 2021; Published Date: October 29, 2021
Citation: Shahzad M, Khan AT, Sandhu Z, Ashraf S, Shariq M, et al. (2021) Digoxin: Decline in Prescribing. J Hosp Med Manage Vol.7 No.9:296 DOI: 10.36648/2471-9781.7.10.296
Introduction
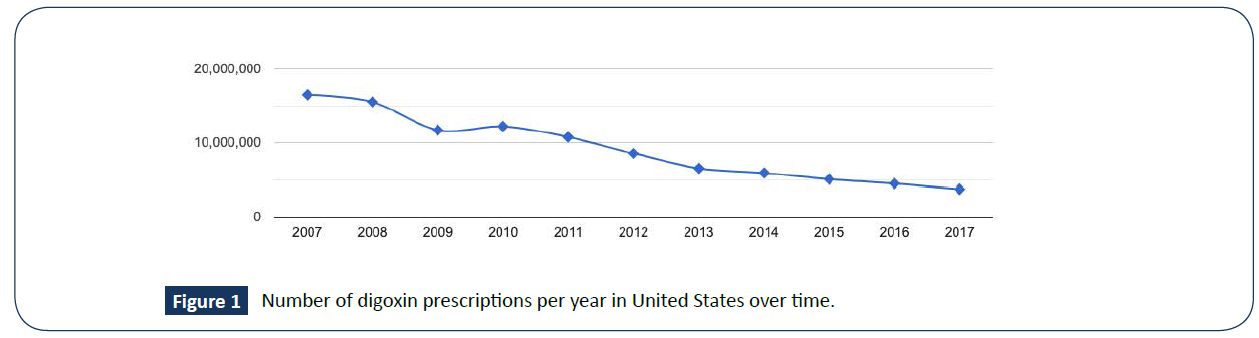
Heart failure is the leading cause of hospital admission [1]. Digoxin is approved for the treatment of heart failure with reduced ejection fraction (HFrEF). The American College of Cardiology Foundation guidelines recommends the use of digoxin, unless contraindicated, to reduce hospitalization due to worsening heart failure in patients with heart failure with HFrEF [2]. Digoxin had been a mainstay of therapy for HFrEF patients and, according to some epidemiologic studies, was the most commonly prescribed drug in heart failure until the late 20th century. According to drug usage statistics in the United States (2007-2017) digoxin was the fourth most commonly prescribed drug in 2007. However, there has been a consistent decline in prescribing digoxin over time, ranking 23rd in 2017 as shown in the graph [3] (Figure 1).
In the DIG (Digitalis Investigation Group) trial, digoxin reduces hospitalisation but it does not impact mortality in patients with HFrEF. This lack of mortality benefit of digoxin along with the emergence of other evidence-based guideline type medical therapies that are proven to lower the risk of hospitalisation and all-cause mortality has led to a decline in the prescribing of digoxin in patients with HFrEF [4].
There have been numerous publications reporting conflicting results regarding the benefits of digoxin in patients with HFrEF. Analysis of the registries, observational studies and secondary analysis of randomised trials done for other purposes have reported increased, decreased or neutral effects on mortality. In the Vale-HeFT trial enrolling patients with HFrEF, there was 28% increase in risk of all-cause mortality and a 35% increase in risk of hospitalisation in patients with digoxin use after adjustment for several confounders [5]. Erath and his colleagues performed a retrospective analysis of 1028 patients receiving either an implantable cardioverter defibrillator (ICD) or cardiac resynchronisation therapy between 1996 and 2010 for primary or secondary prevention of sudden cardiac death. In this study, 43% of patients were receiving digoxin either for the treatment of atrial fibrillation, HFrEF or both, and there was a 65% increase in all-cause mortality in patients receiving digoxin after adjustment for potential confounders [6].
In the African-American Heart Failure trial (A-HeFT trial 2004), 60% of patients were on digoxin [7]. In the ASCEND-HF (Effect of Neseritide in Patients with Acute Decompensated Heart Failure 2011) trial, 27% of patients were on digoxin [8] and 26% of the patients were on digoxin in EMPHASIS-HF (Eplerenone reduced the risk of death and hospitalisation in patient with Moderate systolic dysfunction and NYHA class two symptoms, 2011) trial [9]. In the DAPA-HF trial, 18.8% of the patients were on digoxin.
There has been a decline of digoxin prescribing over the years and at the same time the management of heart failure (HF) has improved with the advent of novel medical therapies. Recent advancements in the management of HF has been as a result of researching the various pathways that lead to the development of heart failure. These pathways have been identified and have been the target of novel HF therapies. Clinicians now have more options to manage HF. Current guidelines recommends beta-blockers, renin angiotensin aldosterone inhibitors and mineralocorticoid receptor antagonists as primary pharmacotherapy in the management of HFrEF, and SGLT2 inhibitors are to be added as secondary pharmacotherapy [10].
A recent study by Malik and his colleagues showed that among hospitalized older patients with HFrEF who are receiving more contemporary guideline-directed medical therapies including ACEi /ARBs, beta-blockers and mineralocorticoid receptor antagonists, the discontinuation of pre-admission digoxin therapy was associated with poor outcomes [11]. This study suggests that digoxin still has a role to play in the management of HF and more prospective studies need to be conducted to study its clinical benefit in HFrEF patients.
In conclusion, digoxin has had a significant impact in the management of heart failure since its inception; yet it has largely been superseded by more contemporary options as the first line choice for heart failure. However, digoxin still has an active role in heart failure and is still often used as an addition to the first-line management in symptomatic HFrEF patients.
References
- Jencks SF, Williams MV, Coleman EA (2009) Rehospitalizations among patients in the Medicare fee-for-service program. N Engl J Med 360:1418-1428.
- Yancy CW, Jessup M, Bozkurt B, Butler J, (2013) 2013 ACCF/AHA guideline for the management of heart failure: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol 62:147-239.
- Kane, SP. Digoxin (2020) Drug Usage Statistics, United States, 2013 - 2019.
- Patel N, Macon C, Thadani U, Schulte PJ (2016) Temporal trends of digoxin use in patients hospitalized with heart failure: analysis from the American Heart Association Get With The Guidelines-Heart Failure Registry. J Am Coll Cardiol 4:348-356.
- Butler J, Anand IS, Kuskowski MA, Rector (2010). Digoxin use and heart failure outcomes: results from the Valsartan Heart Failure Trial (Val‐HeFT). ESC heart failure 16:191-195.
- Erath JW, Vamos M, Hohnloser SH (2016) Effects of digitalis on mortality in a large cohort of implantable cardioverter defibrillator recipients: results of a long-term follow-up study in 1020 patients. Eur Heart J 2:168-174.
- McNamara DM, Tam SW, Sabolinski ML, Tobelmann P (2006). Aldosterone synthase promoter polymorphism predicts outcome in African Americans with heart failure: results from the A-HeFT Trial. J Am Coll Cardiol 48:1277-1282.
- O'Connor CM, Starling RC, Hernandez AF, Armstrong PW (2011). Effect of nesiritide in patients with acute decompensated heart failure. N Engl J Med 365:32-43.
- Zanna F, McMurray JJ, Krum H, Swedberg K, Shi H (2011). Eplerenone in patients with systolic heart failure and mild symptoms. N Engl J Med, 364:11-21.
- Pellicori P, Khan MJI, Graham FJ (2020). New perspectives and future directions in the treatment of heart failure. Heart Fail Rev 21:147-159.
- Malik A, Masson R, Singh S (2019) Digoxin discontinuation and outcomes in patients with heart failure with reduced ejection fraction. J Am Coll Cardiol Title 74:617-627.
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences