Excessive Ancillary Testing by Healthcare Providers: Reasons and Proposed Solutions
Bhardwaj A
DOI10.36648/2471-9781.19.5.52
Bhardwaj A*
Department of Neurology, University of Texas Medical Branch (UTMB), Galveston, Texas, USA
- Corresponding Author:
- Bhardwaj A
Department of Neurology
University of Texas Medical Branch (UTMB)
Galveston, Texas 9.128 John Sealy Annex
Route 0539, 301 University Blvd, Galveston
Texas 77555, USA
Tel: 409-772-8068
E-mail: anbhardw@UTMB.EDU
Received Date: February 20, 2019; Accepted Date: March 13, 2019; Published Date: March 18, 2019
Citation: Bhardwaj A (2019) Excessive Ancillary Testing by Healthcare Providers: Reasons and Proposed Solutions. J Hosp Med Manage Vol.5 No.1:1
Copyright: © 2019 Bhardwaj A. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Abstract
Excessive ancillary testing by healthcare providers pervades clinical practice and is a major cause of mounting healthcare costs. The principal reasons include ubiquitous practice of defensive medicine, widespread usage of inappropriate and obsolete tests, technological advances, patient expectations and demands, and financial rewards for providers. Effective solutions would help lessen the testing-related healthcare cost burden by enhancing awareness of the problem, educating present and future generations of healthcare providers to be costconscious, instituting malpractice liability reform, monitoring test utilization, and focusing on patient education with a shared decision-making model in disease management.
Keywords
Healthcare providers; Patient education; Healthcare costs
Introduction
Healthcare costs in the U.S. have escalated exponentially over the past several decades and are now approaching 20% of Gross National Product (GDP), far more than any other country [1-3]. Runaway healthcare cost growth has widespread ramifications putting enormous pressure on patients and their families, healthcare providers, government, and the economy in general. Further compounding the matter are diminishing reimbursements by third-party payers (i.e., Medicare, Medicaid, and commercial payers). On a macro level, factors that contribute to rising healthcare costs in clinical practice include 1) management of chronic diseases (over 85% of healthcare costs); 2) expensive healthcare technology; 3) payment models such as “fee-for-service”; 4) unregulated and exorbitant pricing of pharmaceuticals and hospital services; 5) fragmented and uncoordinated acute and chronic patient care; 6) high and increasing administrative costs (estimated to be 20-30% of all U.S. healthcare costs); 7) inflated end-of-life care; and 8) excessive ancillary tests and overtreatment [4,5]. Consolidation and mergers of healthcare organizations (HCOs) compound the problem as enhanced market power leads to burgeoning pricing via oligopolistic practices despite economies of scale. More than ever, providing high-quality care (i.e., safe, effective, patientcentered, timely, efficient, and equitable) [1] and enhancing patient satisfaction at a lower cost are becoming critical in U.S. healthcare.
The present treatise provides a broad, literature-based, descriptive overview of the excessive use of ancillary tests as a major driver of healthcare costs. It explores the causes of excessive testing in clinical practice and highlights possible solutions for providing “low cost, high value” healthcare.
Scope of the Problem
Excessive testing is a pervasive problem across the spectrum of patient care, irrespective of type of practice or HCO (private practice, academic institution, etc.), and more so in certain medical specialties. In a national survey of physicians funded by the Robert Wood Johnson Foundation, 73% of respondents characterized frequency of unnecessary tests and procedures as a “serious problem”; 72% responded that they order, on average, one unnecessary test or procedure per week [6]. There are myriad reasons for excessive testing in healthcare. While deriving generally from evolving cultural views on health and disease, the underlying factors include defensive medicine driven by fear of malpractice, concerns about misdiagnosis, deficiencies in medical education and training, inexperience, overreliance on protocols and algorithms, use of incorrect or obsolete tests, advancing technology, patient demands and expectations, lack of cost awareness by healthcare providers, and healthcare insurance and monetary return.
Reasons for Excessive Testing
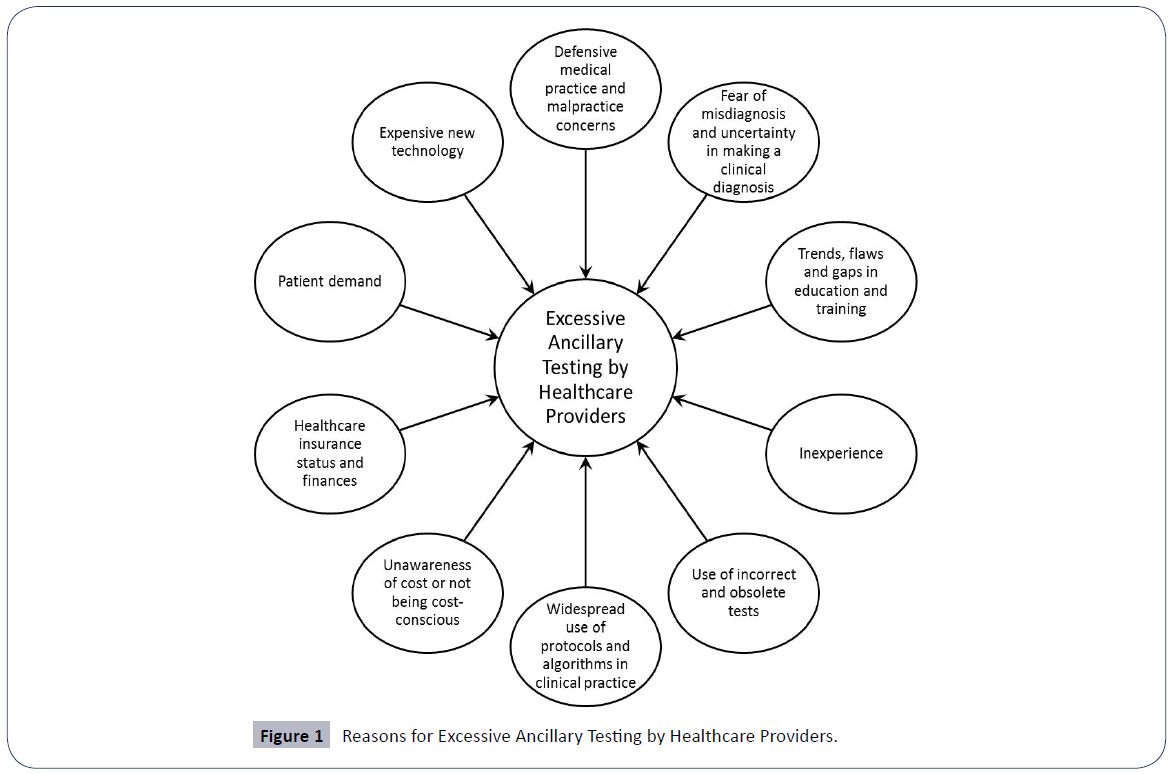
Figure 1 shows Reasons for Excessive Ancillary Testing by Healthcare Providers.
Defensive practice of medicine and malpractice concerns
Defined as “departing from standard medical practice to avoid exposure to litigation,” [7,8] defensive medicine is so common in clinical practice that some have characterized the number and frequency of associated claims and lawsuits as an “epidemic” [7]. Estimates put the cost of medical liability including defensive medicine in excess of $55 billion per year or 2.4% of total healthcare spending [9]. Not surprisingly, data suggests that excessive testing occurs primarily due to fear of litigation over misdiagnosis. Engaging in defensive medicine may significantly alter an individual healthcare provider’s practice and can extend to an entire HCO [7-9]. The proportion of cases actually litigated may be relatively small, with most verdicts favouring the healthcare provider and very few resulting in payment to claimants. And while virtually all healthcare providers carry malpractice insurance, the mere threat of legal action can have profoundly detrimental psychological effects with or without adverse impact on a provider’s professional reputation. Excessive testing by healthcare providers is in large part due to their apprehension, anxiety, and high degree of paranoia stemming from the growing public perception that medical services are “a product with concomitant warranties and guarantees” rendered to “customers” rather than to patients [8,9]. Several reports [9-11] including a survey of primary care physicians reported that 42% of their patients were receiving too much care, with the fear of litigation being the most frequent driver of excessive intervention [12]. This corroborates a study reporting that 52% of physicians order unnecessary tests and procedures out of concern over potential malpractice litigation (6), but without demonstrably better results in terms of patient care [7]. In another study, 92% of physicians ordered imaging tests and other diagnostic measures simply for reassurance [11]. Defensive medicine is more prevalent among private practice physicians (73%) than government-employed physicians (48%). A majority of physicians across specialties tend to adopt a defensive professional stance [13,14], even more so in subspecialties—e.g. 50% of physicians operating in emergency departments were concerned about the possibility of malpractice litigation [15]. Thus, providers in subspecialties that are “high risk” for litigation (e.g., emergency medicine, orthopaedics, obstetrics and gynaecology) find themselves deviating from the proper course of their medical practice. In another survey, 97% of emergency physicians acknowledged ordering redundant advanced imaging scans, a practice equally widespread in academic centers and community hospitals, with 64% of respondents doing so out of malpractice concerns [16].
Fear of misdiagnosis and uncertainty in making a clinical diagnosis
Despite the best efforts of healthcare providers, medicine is predominantly a human endeavor in which mistakes will inevitably occur. Whether among professional colleagues, patients and their families, or the media, there is relatively low tolerance for medical mistakes of commission, but errors of omission may have equally regrettable results. For healthcare providers, the psychological trauma and professional consequences of a misdiagnosis can be dire. Not surprisingly, up to 30% of physicians order unnecessary tests and procedures for the reassurance of having more information. Almost 69% of emergency physicians admit to over-imaging for fear of missing even a low-probability diagnosis [15,16].
Trends, flaws, and gaps in medical education and training
Medical education and training has hitherto aimed to develop clinical skills for the purpose of eliciting a complete history of illness and then formulating a differential diagnosis based on a thorough bedside clinical examination. This aim is being undermined by reliance on ancillary tests that may or may not support the clinical impression. For example, a healthcare provider may simply order an abdominal ultrasound or CT scan for vague abdominal discomfort rather than follow the clinical method of a thorough history-taking and physical exam of the abdomen. Overreliance on imaging for neurological disorders or lower back pain can lead to a “kitchen sink” approach to clinical practice. Moreover, the frequently cited higher sensitivity for such ancillary tests constitutes a weak argument because validation is lacking without thorough bedside clinical methods and outcomes [17].
Inexperience vs. specialization
The practice of medicine is deeply rooted in knowledge accumulated through “pattern recognition” of symptoms, signs, syndromes, and diseases, which is an indirect function of the number of cases encountered as well as duration in clinical practice. For example, a neurologist as subspecialist will be more adept than a general practitioner, internist, or primary care physician in making a clinical diagnosis of a neurological disorder and therefore be less likely to order unnecessary neuroimaging studies.
Use of protocols and algorithms in clinical practice
With the emphasis on “evidence-based medicine” since the 1990s, the development of protocols and algorithms for certain diseases has been encouraged to guide practice and management in reducing variability in patient care. However, a cost analysis on many of such protocols is lacking. Some protocols for improving metrics such as reducing “length of stay” for inpatients may indeed result in cost containment in many instances. Yet while protocolized care and algorithmic management have several advantages, this “one-size-fits-all” approach encourages all patients in a designated category (e.g. transient ischemic attack, acute coronary syndrome, etc.) to undergo ancillary tests, not all of which may be necessary. Data on overall cost-effectiveness for such approaches is limited and further studies are direly needed. Furthermore, routine laboratory tests are often performed on patients admitted to hospital (e.g., daily serum chemistry, complete blood count, coagulation profile, chest radiograph, etc.) without clear underlying clinical indications for doing so. Variation in diagnostic testing among teaching and non-teaching institutions has also been reported, with significantly more diagnostic tests performed in teaching hospitals [18].
Incorrect and obsolete tests
Administering unnecessary tests and using obsolete tests are both omnipresent [19] in clinical practice. Examples of unnecessary tests include bleeding time, IgG food allergy, and sinus computerized tomography (CT) scans for acute rhinosinusitis. The American Academy of Allergy, Asthma & Immunology and the American Society of Clinical Pathology provide guidelines and recommendations for tests that have high yield in particular disorders and clinical scenarios. Examples of obsolete or incorrect tests and some preferred substitutes include 1) C-reactive protein as more sensitive and specific for inflammatory conditions than erythrocyte sedimentation rate (ESR); 2) Troponin I or T for acute myocardial infarction instead of Creatinine Kinase-MB; 3) serum lipase instead of amylase for acute pancreatitis; 4) lecithin/sphingomyelin ratio for fetal lung maturity; 5) qualitative serum human chorionic gonadotrophin (HCG) for pregnancy; 6) Prostatic Acid Phosphatase for prostatic cancer; and 6) serum or red cell folate [19]. Imaging with non-contrast versus contrastenhanced studies (CT or Magnetic Resonance Imaging) is frequently incorrectly performed for certain disorders leading to repeat testing and subjecting patients to the deleterious effects of needless exposure to radiation and contrast material. Predictably, “excessive testing begets more testing,” whereby one test demonstrates an abnormality necessitating a second test for justification and further investigation with potential harm and little benefit to the patient [20]. Incidental findings on tests that do not correlate with symptoms and signs frequently warrant even more testing for clarification.
Technological advances
Over the past three decades, technological advances leading to the rapid development of newer diagnostic techniques (e.g., biomarkers, genetic testing, neuroimaging, etc.) have enhanced medical practitioners’ ability to confirm clinical impressions and diagnoses in ways previously thought not possible. Providers are increasingly turning to such tests because they are readily available to confirm or rule out a clinical impression. Data on the cost effectiveness of such expensive diagnostic testing is limited. In the inpatient setting, portable CT scanners housed in close proximity to intensive care units (ICUs) are being utilized with greater frequency to substitute for a thorough bedside examination. Patients in the ambulatory setting often request a particularly expensive test to allay their fears of a genetic or neurodegenerative disorder (e.g. PET scans and amyloid imaging for dementias and Alzheimer’s disease) or rule out an ominous “diagnosis” based on an Internet search. Screening and testing for rare genetic disorders is extremely expensive and the costs are not covered by third party payers.
Patient demands and expectations
In general, demand for testing by patients is becoming increasingly widespread. In the physician survey [6], patients’ insistence comprised 28% of the reasons for testing, with 23% being done to “keep patients happy.” Some patients lose confidence in their healthcare providers when told that certain testing is not required and may even go “doctor shopping” if their belief that testing is needed goes unaddressed. Evolving societal values are altering expectations regarding health and disease in conjunction with lessening confidence in healthcare providers thanks to easy access to web-based information and advertising. While healthcare providers are bound to follow the tenets of the Hippocratic Oath in treating disease and alleviating pain and suffering, patients’ views on longevity and quality of life are increasingly challenging the traditional assumption that “life is ephemeral.” Patient demand for more testing is having very real effects. Almost 50% of primary care physicians are more likely than specialists (40% versus 24%) to have patients request unnecessary tests or procedures at least several times per week [6]. And up to 87% of physicians talk to their patients about reasons to avoid a test or procedure when a patient requests one [6]. This could have an impact on provider ratings by patients that is increasingly being utilized in value-based reimbursement models.
Unawareness of cost or not being cost-conscious
Failure to learn about the business aspects of healthcare during undergraduate (medical school, etc.) and post-graduate (fellowship) training results in many providers not being costconscious or simply being ignorant of healthcare costs. The mindset and focus on “doing the best for the patient irrespective of cost” along with the resulting operational framework becomes ingrained in their day-to-day clinical practice. Some healthcare providers may rationalize not being cost-conscious because they feel it is difficult or perhaps even unethical to evaluate human disease and suffering in monetary terms.
Healthcare insurance status and financial incentives
It is common practice for healthcare providers to make decisions on ancillary testing based on insurance coverage (by third-party payers, co-payments, etc.). Patients with private insurance who are admitted to hospital stay much longer and are subject to far more testing and procedures than patients without health insurance [13]. Presently, the majority of reimbursement for testing for in-patient services is bundled in diagnosis-related group (DRG)-based payment models. However, interpretation of these tests is based on fees-for-service for physicians indirectly incentivize more testing in a productivity-based model for physician compensation. If insurance bundles the technical and the healthcare provider component, a provider may understandably opt for a less expensive test.
Proposed Solutions
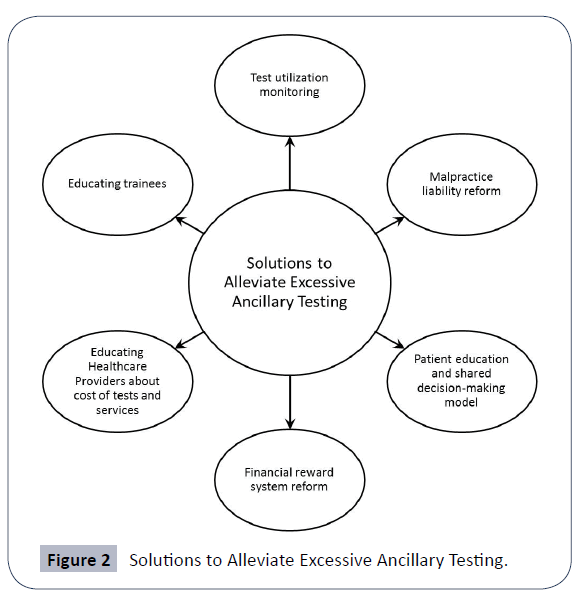
Figure 2 shows Solutions to Alleviate Excessive Ancillary Testing.
The majority of healthcare providers believe that excessive testing in clinical practice is a serious problem. Two-thirds (66%) of physicians feel a responsibility to ensure that their patients avoid unnecessary care, and 58% of physicians feel that they are well-positioned to address the issue. In a literature-based review, a majority of interventions to improve physicians' testing practices claimed success, with interventions focused on multiple behavioral factors being more successful [20,21]. Education, technical approaches, real-time feedback and peer comparison are all needed to drive change.
Test utilization monitoring
Tests impact patient health by modulating diagnostic and treatment decisions, affecting time to treatment, modifying healthcare provider practice and patient perceptions, or by exposing patients to risk [17]. The accuracy of a test is not always a necessary prerequisite for improved patient outcomes. Appropriate tests should be utilized only after carefully evaluating their value (including cost/benefit) by assessing patient outcomes. Moreover, all tests must be ordered based on pretest probability and interpreted as such.
Use of peer management [22] through a “resource utilization committee” or a “test utilization oversight” mechanism by HCOs can facilitate focus on cost-containment while providing safe and effective reductions in unnecessary clinical laboratory testing [23]. Laboratory testing stewardship formulation with teams or “dyads” including hospital administrators is being incorporated in certain HCOs with encouraging results [24]. Some of the methods that can be used include creating awareness of the problem, forbidding certain tests, developing a laboratory test oversight committee, prohibiting repetitive orders, granting special privileges for ordering providers, requiring higher-level approval, refining computerized test menus, utilizing score cards for laboratory testing, programming reminders (“pop-ups”) to avoid repeat testing, and educating healthcare providers [25]. In addition, third party payers may refuse to pay for tests deemed in excess or may augment the need for pre-authorizations for certain tests [20]. Inevitably, requiring pre-approval for tests by third-party payers will become more common in the future. Such efforts as Choosing Wisely [26], an initiative of the ABIM Foundation with input from over 30 medical specialties, have identified frequently used tests whose value is questionable including 1) screening for cervical cancer in women aged > 65 years deemed not at high risk; 2) screening for carotid occlusive disease in asymptomatic patients; 3) CT or MRI of brain in patients presenting with syncope with normal neurological examination [20]. Implementation of Choosing Wisely and multimodal quality improvement measures (healthcare provider education, electronic health record redesign, audit, and feedback), has resulted in substantial reductions in the over testing of blood chemistries in emergency rooms [27]. Similarly, refinement of existing protocols has resulted in decreased routine laboratory testing and imaging in elective preoperative evaluations without increases in adverse events [28].
Futuristic-minded healthcare providers may envision technological advances leading to “whole body scans” as screening tools for rapidly and accurately diagnosing disease and as being particularly useful for early diagnosis. Although advances in testing may eventually supplant the conventional clinical methods of thorough history-taking, physical examination, and differential diagnosis formulation deemed “archaic” by some, it is imperative to remain cost-conscious as these newer diagnostic approaches will likely further drive up the cost of healthcare. The true value of any new test must be critically evaluated in terms of its impact on health and disease management.
Malpractice liability reform
The fear of missing a diagnosis and of a resulting malpractice lawsuit impels many healthcare providers to order several tests without always critically assessing their relative benefits. Studies on cost saving from malpractice liability reform have been inconsistent. While some have suggested that estimated savings from decline in medical malpractice premiums would result in minimal reduction in total medical care costs [29]. Others suggest that fears of malpractice lawsuit are allayed in states with tort reform resulting in a more considered approach to diagnosis and disease management. Ninety-one percent of physicians suggest that malpractice reform would be an effective way to reduce unnecessary tests and procedures. Seventy-nine percent of emergency physicians reported that malpractice reform would lower rates of excessive imaging testing [14]. It has been suggested that healthcare providers could counter their fear of being litigated if they would assess the actual risk of a malpractice suit in their specific sub-specialty and location of practice [9]. Frequently, the actual risk is lower than the perceived risk.
Patient education and the shared decisionmaking model
Proactive communication with patients and their families to address the risks and benefits of invasive and noninvasive tests is critical. Healthcare providers must communicate honestly, taking ownership of errors and presenting alternatives to patients by setting aside time to do so. Eighty-five percent of physicians indicate that specific, evidence-based recommendations that they can offer their patients would be helpful in reducing excessive testing, and up to 78% said that having more time to discuss alternatives with patients would be effective (6). Resources available to healthcare providers to further help in decision-making include Dartmouth-Hitchcock’s Center for Shared Decision Making [30].
Reforming the system of financial rewards
Sixty-one percent of physicians say that changing the system of financial rewards (fee-for-service) some physicians receive for ordering tests and procedures would be an effective solution [6,31,32]. Bundled payments for DRG-based testing of patients admitted to hospital would help reduce excessive testing [31].
Educating trainees
While training for medical students, residents, fellows and healthcare trainees is evolving rapidly along with technological advances (e.g. simulation techniques, etc.), the shift toward increased dependence on ancillary testing in formulating a diagnosis over the last few decades has also been significant. In addition, time constraints and increased demands for documentation play a big role in decreasing time for the traditional clinical methods of meticulous history-taking and thorough physical examination to formulate a differential diagnosis with subsequent corroboration by confirmatory tests. To provide optimal high-value care to patients, it will be critical to maintain this thoughtful methodological approach toward making a diagnosis.
Educating healthcare providers about cost of tests and services
Healthcare providers at all levels must be educated and wellinformed about the cost of patient care (e.g., tests, drug pricing, etc.). As providers learn the basics of healthcare finances and marketing, they should become more “cost conscious,” enhancing the judicious use of ancillary testing and underscoring the collective responsibility to drive down the costs of healthcare. In a prospective study, both administrative interventions (i.e., restricting available emergency laboratory tests and frequency of repeated orders) and educational interventions (i.e., discussions with hospital medical staff and presentation of the new restrictive policy) resulted in an almost 20% reduction over a one-year period in clinical biochemistry and haematological testing in inpatients at a teaching hospital (25). Courses on the cost of healthcare must be incorporated into medical school and postgraduate residency training curricula. Professional medical societies should expand their roles as well by instituting online and face-to-face courses on this topic at their regional and national meetings.
Conclusions and Future Directions
The tendency to perform unnecessary and excessive ancillary tests is highly prevalent in clinical practice, a problem involving the key stakeholders in healthcare—patients, providers, and third-party payers. The reasons underlying this ubiquitous trend include malpractice concerns, a desire by healthcare providers to reassure themselves of a clinical diagnosis, and responding to patient demands. An effective way of addressing the problem would be to implement specific, evidence-based indications and recommendations for ancillary tests. Enhancing awareness and encouraging healthcare providers to be more receptive to costcontainment through more thoughtful and judicious performance of ancillary diagnostic tests while maintaining a focus on quality metrics such as patient satisfaction and outcomes will benefit HCOs in becoming higher-value organizations.
References
- Building Constructive Hospital/Medical Staff Relationships and Alignment. The Walker Company Healthcare Consulting, BoardBrief.
- White KR, Griffith JR (2010) The well-managed healthcare organization. 7th Edition, AUPHA, Chicago, Illinois, USA.
- Becker’s CFO Report (2014) 9 Drivers of high healthcare costs in the U.S.
- Taube S (2016) What is Driving Rising U.S. Healthcare Costs?
- Rosenthal E (2014) Medicine’s Top Earners Are Not the M.D.s. The New York Times.
- PerryUndem (2014) Unnecessary tests and procedures in the Health Care System. What physicians say about the problem, causes, and the solutions. Results from a National Survey of Physicians. Conducted by the ABIM Foundation. Sponsored by the Robert Wood Johnson Foundation.
- Sekhar MS, Vyas N (2013) Defensive Medicine: A Bane to Healthcare. Ann Med Health Sci Res 3: 295-6.
- Hauser MJ, Commons ML, Bursztajn HJ, Gutheil TG (2016) Fear of malpractice liability and its role in clinical decision making. In Gutheil TG, Bursztajn HJ, Brodsky A, Alexander V (Eds.), Decision making in psychiatry and the law (pp. 209-226). Baltimore, MD, US: Williams & Wilkins Co.
- Mello MM, Chanra A, Gawande AA, Studdert DM (2010) National costs of the medical liability system. Health Aff (Millwood) 29: 1569-1577.
- Carrier ER, Reschovsky JD, Katz DA, Mello MM (2013) High physician concern about malpractice risk predicts aggressive diagnostic testing in office-based practice. Health Aff (Millwood) 32: 1383-1391.
- Jena AB, Seabury S, Lakdawalla D, Chandra A (2011) Malpractice risk according to physician specialty. N Eng J Med 365: 629-636.
- Sirovich BE, Woloshin S, Schwartz LM (2011) Too little? Too much? Primary care physicians’ views on US health care: a brief report. Arch Intern Med 17: 1582-1585.
- Studdert DM, Mello MM, Sage WM, Des Roches CM, Peugh J et al. (2005) Defensive medicine among high-risk specialist physicians in a volatile malpractice environment. JAMA 293: 2609-2617.
- McClellan MK (1996) Do doctors practice defensive medicine? QJ Econ 11: 353-390.
- Rodriguez RM, Anglin D, Hankin A, Hayden SR, Phelps M et al. (2007) A longitudinal study of emergency medicine residents’ malpractice fear and defensive medicine. Acad Emerg Med 14: 569-573.
- Kanzaria HK, Hoffman JR, Probst MA, Caloyeras JP, Berry SH et al. (2015) Emergency physician perceptions of medically unnecessary advanced diagnostic imaging. Acad Emerg Med 22: 390-398.
- Ferrante di Ruffano L, Hyde CJ, McCaffery KJ, Bossuyt PM, Deeks JJ (2012) Assessing the value of diagnostic tests: a framework for designing and evaluating trials. BMJ 344: e686.
- Spence J, Bell DD, Garland A (2014) Variation in diagnostic testing in ICUs: a comparison of teaching and nonteaching hospitals in a regional system. Crit Care Med 42: 9-16.
- Wu AHB, Lewandrowski K, Gronowski AM, Grenache DG, Sokoll LJ, et al. (2010) Antiquated Tests Within the Clinical Pathology Laboratory. Am J Manag Care 16: e220-e227.
- Cruz JS (2018) Minimizing fear-driven diagnostic testing. Today’s Geriatric Medicine.
- Solomon DH, Hashimoto H, Daltroy L, Liang MH (1998) Techniques to improve physicians’ use of diagnostic tests: A conceptual framework. JAMA 280: 2020-2027.
- Neilson EG, Johnson KB, Rosenbloom ST, Dupont WD, Talbert D, et al. (2004) Resource Utilization Committee. The impact of peer management on test-ordering behavior. Ann Intern Med 141: 196-204.
- Konger RL, Ndekwe P, Jones G, Schmidt RP, Trey M, et al. (2016) Reduction in Unnecessary Clinical laboratory testing through utilization management at a US Government Veterans Affairs Hospital. Am J Clin Pathol 145: 355-64.
- Bhardwaj A (2017) Alignment between physicians and hospital administrators: historical perspective and future directions. Hospital Practice 45: 81-87.
- Baird G (2014) The laboratory test utilization management toolbox. Biochem Med (Zagreb) 24: 223-34.
- Choosing Wisely (2018) Promoting conversations between patients and clinicians.
- Venkatesh AK, Hajdasz D, Rothenberg C, Dashevsky M (2018) Reducing Unnecessary Blood Chemistry Testing in the Emergency Department: Implementation of Choosing Wisely. Am J Med Qual 33: 81-85.
- Nelson SE, Li G, Shi H, Terekhov M, Ehrenfeld JM, et al. (2018) The impact of reduction of testing at a Preoperative Evaluation Clinic for elective cases: Value added without adverse outcomes. J Clin Anesth 55: 92-99.
- Thomas JW, Ziller EC, Thayer DA (2010) Low costs of defensive medicine, small savings from tort reform. Health Affairs 29: 1578–1584.
- Dartmouth-Hitchcock’s (2018) Center for Shared Decision Making.
- Birbeck GL, Gifford DR, Song J, Belin TR, Mittman BS et al. (2004) Do malpractice concerns, payment mechanisms, and attitudes influence test-ordering decisions? Neurology 62: 119-21.
- Calderon-Margalit R, Mor-Yosef S, Mayer M, Adler B, Shapira SC (2005) An administrative intervention to improve the utilization of laboratory tests within a university hospital. Int J Qual Health Care 17: 243-248.
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences