Hospital Bed Occupancy and Utilisation: Is Kuwait on the Right Track
Kelendar H and Mohammed MA
DOI10.36648/2471-9781.19.5.59
Faculty of Health Studies, University of Bradford, Bradford, UK
- *Corresponding Author:
- Hisham Kelendar
Faculty of Health Studies
University of Bradford, Bradford, UK
Tel: 07473836045
E-mail: dr.hisham81@gmail.com
Received Date: October 13, 2019; Accepted Date: November 13, 2019; Published Date: November 30, 2019
Citation: Kelendar H, Mohammed MA (2019) Hospital Bed Occupancy and Utilisation: Is Kuwait on the Right Track? J Hosp Med Manage Vol.5 No.2:3
DOI: 10.36648/2471-9781.5.2.46
Abstract
Purpose: Before taking decisions to add more beds and expand by providing health services, the decision makers should analyse the existing bed capacity in terms of the demographic distribution, subspecialties allocation, the occupancy rate and patient length of stay. Furthermore, they are required to appreciate the best possible way of utilising their existing assets effectively and efficiently. In this era, the aim of this article is to explore the different aspects affecting the hospital bed capacity in the literature. Followed by analysing the current situation of the hospital bed occupancy and utilisation in Kuwait and how far it is from other developed countries. Design/Methodology/Approach: Through conducting a literature review, an exploration of the different aspects affecting the hospital bed capacity and analysing the current situation of the hospital bed utilisation in Kuwait and how far it is from other developed countries will be achieved. By using a documentary review research method, secondary data will be approached using the national statistical references provided yearly by Kuwait’s MOH. The international statistics will be approached through reviewing NHS England, the Organisation for Economic Cooperation and Development and USA databases and their publications electronically from their official websites. Findings: In Kuwait, expenditure in the healthcare services is increasing year after year and is expected to double within 5 years, if we consider the statistics of the last 10 years. Currently, 10 mega projects worth approximately 2 billion KD are being constructed in Kuwait. In comparison to 2013, where the total bed capacity of the governmental sector was 6663, the number of beds is expected to reach 13474 in 2020. This means that the bed capacity is expected to be doubled by adding 6772 beds. This decision is considered a big challenge especially with 63.6% average occupancy rate between the period from 2006 to 2015. Kuwait’s MOH should consider all the previous data for their future planning especially with the decision of adding more beds. Even with the low hospital bed occupancy rate in comparison to Europe countries, Kuwait’s government has taken the decision to expand their bed capacity in the next few years. One way to lower the bed cost is to improve and enhance their utilisation. Lean philosophy could have an essential role in enhancing the utilisation of the existing bed capacity and planning for any future requirements. Therefore, inappropriate usage of the existing beds is considered as a main factor that affects their efficiency. Originality/value: It is time to raise the following question: is there a requirement to add excess capacity in Kuwait’s healthcare organization? and if so, from economic analysis, what is the cost of that excess capacity and how will it be reflected on the quality of services. The decision of expanding an organisation’s bed capacity and infrastructure required bringing together all key stockholders under one umbrella and adopting analytical strategies that helps in making the right decisions considering the allocation and use of the existing hospital beds and added extra beds where it is required in order to have an efficient service. This paper highlights lean as an approach of optimising the use of the existing resources and managing the bed occupancy in an efficient way. In addition, the article explores the different factors that affect the decision of expanding the organization’s bed capacity and the influence of empty beds. Kuwait’s MOH requires more in-depth studying regarding the idea of adding more beds while examining their implication on different aspects. Policy makers are required to have a sustainable system and balancing between the supply and demand in the best possible way, to achieve an efficient productive system.
Keywords
Hospital beds; Efficiency; Demand; Bed capacity; Bed utilisation; Lean
Introduction
The upsurge in healthcare costs, the increase in healthcare services demand and health reform, are key issues discussed among politicians and the community in general. There is a high interest and demand for greater operating efficiency reform in order to provide better healthcare outcomes with lower costs [1]. Since the 1980s, there is extensive literature about hospital resources management and capacity planning [2-5]. One of the main interested areas for many studies was about the cost of excess capacity or the cost of empty hospital beds [6-9]. The cost of empty hospital beds emerges as an important public policy issue and as a justification for the health planning program [8]. The beds inside the hospital are considered as vital medical equipment [10]. The management of the bed capacity will have an effect on the quality, expenses and the accessibility of all care [11]. The cost associated with empty beds represents wasteful expense. Furthermore, the inappropriate bed occupancy rate is considered a waste of resources [12,13]. Many developed countries, mainly in the USA and Europe, started to use the reduction in their total beds capacity as measures to restrict hospital expenditure [14,15]. The main concerns, in most of the countries’ governments that initiate the idea of hospital bed reductions, is the rising costs in the healthcare sector [14]. They implemented a different strategy to use the existing resources efficiently and effectively in order to minimise the inevitable consequential effect of the bed capacity reduction. On the other hand, developing countries such as Kuwait are on track for expanding their total bed capacity as part of their health reforms [16]. Before taking decisions to add more beds and expand in providing health services, the decision makers should analyse the existing bed capacity in terms of the demographic distribution, subspecialties allocation, the occupancy rate and patient length of stay (LOS). Furthermore, they are required to appreciate the best possible way of utilising their existing assets effectively and efficiently. In this era, the aim of this article is to explore the different aspects affecting the hospital bed capacity in the literature. Followed by analysing the current situation of the hospital bed occupancy and utilisation in Kuwait and how far it is from other developed countries.
The article starts with an explanation of the research methodology, followed by discussing the hospital excess capacity dilemma. Furthermore, a clarification regarding the hospital bed occupancy rate and bed capacity will be provided. Then the author will talk about factors affecting hospital bed occupancy and planning. The Kuwaiti case will be the next section. After that, the highlight will be on lean as an approach for improving hospital bed utilisation. Finally, the limitations, conclusion and future research will be mentioned respectively.
Methodology
Through conducting a literature review, an exploration of the different aspects affecting the hospital bed capacity and analysing the current situation of the hospital bed utilisation in Kuwait and how far it is from other developed countries will be achieved. The author will explore the vast majority of healthcare databases including MEDLINE, CINAHL, Google scholar, Embase and Cochrane Library. The inclusion criteria followed for the reviewed articles involved in this research are to be written in English, published in peer- review, using the previously mentioned database. The keywords include hospital bed, efficiency, demand, bed capacity, bed utilisation, lean, bed occupancy, hospital capacity, Kuwait, hospital planning. After that, all the reference lists of the articles found were reviewed. The initial search reveals 583 articles. After reviewing the titles and the abstract carefully, only 84 articles were related to the topic. Furthermore, following the snowball method, this added another 18 articles. After excluding the duplication and unrelated articles, the net results found 49 studies.
By using a documentary review research method, secondary data will be approached using the national statistical references provided yearly by Kuwait’s Ministry of Health (MOH). The documentary review research method is considered as good as other methods such as interviews, surveys or participant observation and even sometimes more cost-effective [17,18]. It means to review and analyse certain documents about the phenomenon that the researcher attempts to discover [18]. The documentary review is a useful method for translating existing archives and data into general concepts [19]. Ahmed [17] stated that “many researchers state that document researches include institutional memoranda and reports, census publications, government pronouncements and proceedings, diaries and innumerable other written, visual and pictorial sources in different forms and so on”. The researcher will use MOH documents to review the demographic profile, the nature of diseases among the Kuwaiti population, the infrastructure, human resources and the funding sustainability of Kuwait’s Healthcare System (HCS). The documents include the policies, the plans, ministerial decrees the existing data and statistics of Kuwait’s MOH. Some of these documents can be accessed online and some of them as hard copy and no permission were required. The areas of concentration are:
• MOH total bed capacity and the bed occupancy rate (reviewing Kuwait health documents, a statistical book produced annually by MOH, in the last 10 years).
• The future healthcare building project (reviewing MOH for Engineering and Projects department documents).
• The demographic profiles (reviewing Kuwait health documents, a statistical book produced annually by MOH, in the last 10 years).
• Human resources (reviewing The Manpower Statistic annual report in the last 10 years).
The international statistics will be approached through reviewing NHS England, The Organisation for Economic Co-operation and Development (OECD) and USA databases and their publication electronically from their official websites. The hospital beds data from Kuwait will be compared with the data published internationally, specifically within the developed countries.
The hospital excess capacity dilemma
Significant changes occur in the role of the hospital, which leads to putting hospital reform on the higher agenda of the healthcare policy maker. The escalating changes in different perspectives including epidemiology, demographic and technological, with the political constraints, reflected on the pattern of clinical care provided and have forced the changes in the hospital’s organization. Hospitals account for almost 40% of all health care expenditure, which is considered as the largest single source of healthcare costs [20]. By reassessment of the total number of beds required to serve the target population, several hospitals over the world have engaged in various cost-cutting efforts [20]. Reducing the number of acute beds was a trend followed by the US and most European countries for years to increase hospital efficiency [21]. In the USA for example, as presented in Table 1, the total number of hospital beds has been declining substantially.
Table 1 Total beds in U.S. Short-Term Hospitals.
| Year | Beds |
|---|---|
| 1979 | 983,694 |
| 1980 | 988,387 |
| 1981 | 1,003,435 |
| 1982 | 1,012,191 |
| 1983 | 1,018,482 |
| 1984 | 1,017,057 |
| 1985 | 1,000,678 |
| 1986 | 978,275 |
| 1987 | 958,312 |
| 1988 | 946,697 |
| 1989 | 933,318 |
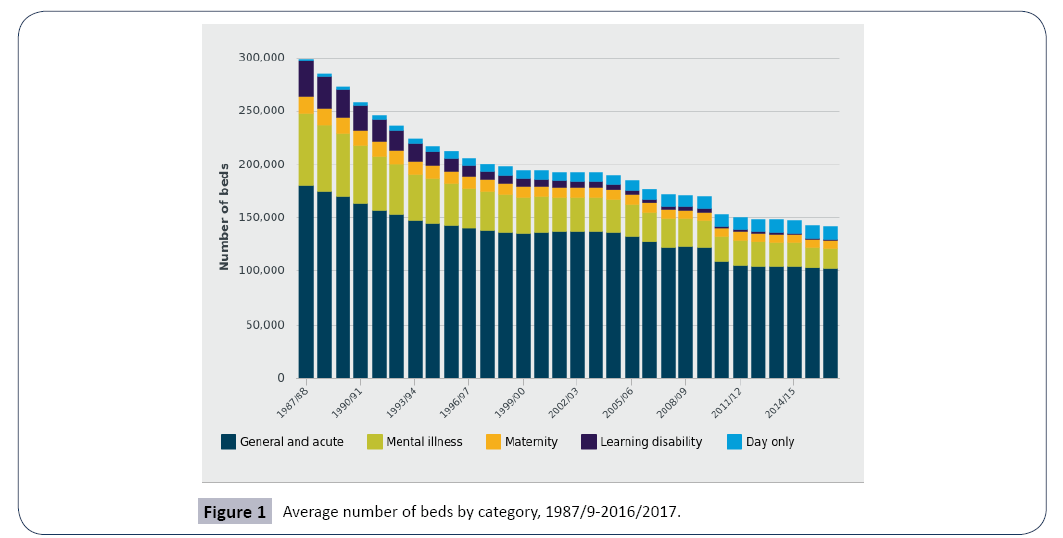
A reduction of 70,000 beds happened between 1983 (1,018,482) and 1989 (933,318) [7]. A more recent statistic from the NHS shows a substantial fall in bed numbers over the past 30 years [22]. Between 1987/8 and 2016/17 the rate of change in bed numbers can be seen in Figure 1. From 300,000 beds in 1987/1988 to approximately 150,000 beds in 2011/2012 almost 50% reduction in the total number of NHS beds within 24 years.
Even though the demand for beds increases with time, mainly in the nations characterised by growing populations, coping with this reduction could be explained by introducing technology that reduces the hospital rooms demand. Technology also, plays a significant role to reduce the average LOS [23]. Furthermore, several diseases and procedures, which required patient admission, could be dealt with as an outpatient treatment. This motivates the decreased use of inpatient care and increases the use of outpatient care, which minimises hospitalisations. These are some factors that helped different countries in their attempt to reduce their total bed capacity. The insufficient number of available beds is not always due to financial reasons, but poor resource management is an important cause.
Empty unused beds can be a result of inefficient management, but at the same time could be a rational response to demand uncertainty [24,25]. As empty beds are a problem, overcrowded hospitals are also considered a big problem. When a patient arrives at the hospital and is required to be admitted, he/she will be expected, since decisions are made that the bed is available for providing her/him with medical treatment. In the healthcare system, where services are provided by the government or what is called free market healthcare, it is a critical issue to have a situation where the patient was not admitted due to lack of capacity. It will be a hot topic for the media, politicians and the community in general. However, the availability of hospital beds by itself could be a cause of additional bed utilisation. This concept was clarified [26] when he said “A built bed is a filled bed”. Indeed, both the over utilised beds and underutilised beds are prevalent problems. In the hospital, it is vital to ensure equilibrium between having a sufficient number of beds so that no patients should be refused and at the same time not to have too many empty beds. This is not an easy task, especially in a complex system such as healthcare that is characterised by different subspecialties, increased demand, large variability of patient and unpredicted numbers of attended cases.
The hospital bed occupancy rate and bed capacity
The hospital capacity is measured by the total number of inpatient beds and the decisions of hospital bed capacity made based on target occupancy levels. Usually, the hospital capacity utilisation is measured by the hospital bed occupancy rate. Historically, the most commonly used occupancy target is 85 per cent, where this optimal occupancy figure could be used for estimating the number of excess beds [27]. This figure is applicable on the hospital in general where specialised units such as intensive care units, that are characterised by high costs, are usually run at much higher utilisation levels [10]. Indeed, because of increased financial pressures, some of the large hospital’s managers have put even higher target levels [20]. The target bed occupancy in France for example, is 85% in medicine and surgery and 95% in obstetrics [28]. Since, the healthcare sector is characterised by uncertain bed demands and patient’s lengths of stay, hospitals are required to operate at less than 100 per cent utilisation. Hence, there is no agreed definition for the optimal bed occupancy level and the percentage of excess capacity that hospitals should have. [29] defined the optimal number of beds as “the number for which the following three criteria are met: the number of unoccupied beds is not excessive (productivity), the number of patients transferred because of full bed occupancy is not excessive (security), and one or perhaps several beds are available for unscheduled admissions (accessibility). A score is constructed based on these three parameters”
The key factors used in calculating the bed capacity are population, length-of-stay, frequency of hospital admission, and bed occupancy [30]. Based on the previous factors, the following formula is developed:
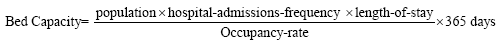
The bed occupancy rate, which is the fraction of time a bed is occupied, is a key indicator used in hospital-capacity planning [30]. It is calculated as:
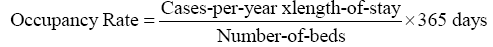
The target bed occupation is a common method used to acknowledge hospital activity and to define hospital bed capacity [28,31]. But it is worth noting that occupancy rate is not the only indicator that should be used for in hospital-capacity planning. Further discussion can be found in the next section about the different approaches used for hospital-capacity planning.
Approaches and factors affecting hospital bed occupancy and planning
Several approaches could be used to determine the required number of beds for each hospital department. One of the common and simple approaches that different medical authorities use is the ratio method, which is based on a census quantifying the number of patients [32-36]. The critics for this model state that it does not consider the fluctuation of requested admissions over time [29]. Moreover, as in the ratio method, the average LOS is used, it overestimates the required beds number for the departments characterised by high average lengths of stay. The hospital facilities utilisation varies during the year even during the week. For example, most elective patients are admitted during weekdays, not on the weekends and very few procedures are scheduled for weekends. Similarly, variability in demand for hospital beds is affected by different seasons of the year and is far from uniform. The demand for hospital beds is lower during the summer and holiday periods [37] and even the different seasonal periods have different effects on different departments. Consequently, the reported bed occupancy rate is usually presented by the yearly averages and do not reveal, meaningfully, the fluctuation of bed occupancy across the year [10]. Furthermore, [10] mentioned that besides targeting occupancy levels for planning bed capacity, it is required to consider measuring the patient delays. Causes of patient delay include but are not limited to: patient waiting time [38], patients refused admission rate [39], patient misplacement [40] and surgery cancellation [41]. As can be seen, planning hospital beds is not an easy task as both demand and LOS have the potential for change. The decision of hospital capacity is also influenced by demographic factors, hospital location, size, and service mix [42]. Therefore, to plan and evaluate bed capacity, it is not enough to rely only on occupancy levels. Other methods used for hospital bed capacity planning and assessing operational performance are related to queuing analysis and simulations (For further deateails see) [43].
The appropriate approach for capacity planning required is an examination of the entire process of patient flow starting from the patient’s arrival in the emergency department to placement in a bed, until discharged with considering different scenarios. A study [44] revealed “In the context of population aging, forecasting the number of hospital beds should not rely on a unique scenario. Using different hypotheses about admission rates and LOS and comparing projected versus real use are important to avoid shortage of bed”. An example of a patient’s path, considering only the main steps, starts from entering the hospital emergency department, towards the reception for registration, then triage where a nurse categorises the patient’s condition. Afterwards, the patient will be seen by an emergency physician, which usually requests the patient to do diagnostic testing such as a blood test. A nurse or technician will collect the laboratory specimens and they will be sent to the hospital’s central lab facility. In case the diagnostic test is required to be done in another location, transport personnel could be needed. When the test results are available, the treating physician will review the results to determine if the patient needs an admission to the hospital. In the case that patient admission is required, a bed will be prepared for the patient in the appropriate unit (e.g., surgical, medical, intensive care….) depending on availability that is related to ward capacity. Indeed, the capacity of the relevant unit is not the only factor that affects the availability of a bed, especially in surgical departments, but also the elective patient admission and scheduling policies, the transfer and discharge policies and procedures [45] and the way of managing the existing bed capacity. If the bed is vacant, cleaned, and the nurses are available, the patient will be moved to the assigned bed. This one scenario of a patient admission process shows the complexities of planning and managing hospital capacity.
Different actors playing roles depend on each other in terms of the bed utilisation and occupancy rate. These include: hospital management or a higher authority that provides the facilities required for patient hospitalisation, patients whose life behaviours influence the medical service demand and physicians who decide if the patients require hospitalisation and their LOS [14]. The relationship between the different actors, especially the hospital management and physicians, govern whose incentives prevail. In Europe, for example, the relationship between physicians and the hospital is either as salaried employees with the hospital, similar to the case studied in this article (Kuwait), or the physicians hire hospital’s facilities as independent entrepreneurs. As in a study [46] indicated, the hospital formal power over the salaried employees physicians is more, than when they are independent entrepreneurs.
A no less important factor in planning hospital bed capacity is the average demand on beds. Indeed, the bed requirements of day-to-day variations in demand will affect the estimation of the average level of demand. Uncertainty, over demand for the healthcare services and variability in the number of patients arriving, in any given time period are a key feature of the hospital environment [8] that affects hospital bed occupancy and planning. The hospital care demand variability can be divided into in two categorises, predictable variations in demand— such as weekends and holidays (seasonal effects), or due to demographic or technological reasons (long-term trends)— and unpredictable variations [47]. The higher percentage of variability is caused by the emergency services, where the demand is difficult to forecast in advance [48]. The reasons behind the demand fluctuations arise from the unpredictable patient lengths of stay and the hospital admission rates [39,49]. A study [8] revealed that the higher variation in forecast hospital demand, the higher the costs. This indicated that hospital costs are affected by demand uncertainty. A study [50] on 43 Portuguese NHS hospitals to evaluate the impact of demand uncertainty on hospital costs. They found that hospitals which experience higher demand uncertainty will have higher excess capacity and significantly higher costs. Since different organizations aim to satisfy demand and reduce the probability of not having adequate capacity, they build excess capacity, which will be associated with more costs.
It is also vital to consider the patient management profile, which has a direct influence on the bed occupancy. Within the hospital, every specialty has their own protocols, management guidelines and operation process, which could explain the practice variation across hospital departments. Further, a study [29] mentioned that “differences result from the constraints imposed by sitespecific characteristics of patient recruitment and the structural, organizational, geographical, historical and political environment in which the hospital operates” which could determine the number of beds. It is worth noting that the previous factors overlap, and sometimes one factor affects the other factors either directly or indirectly. The patient admission policy can affect the patient demand and at the same time the demand can influence the admission’s policy and bed utilisation. The patient admission policies “deal with controlling patient demand and -mix through combinations of elective, waitlisted, and emergency admissions, and within-hospital patient transfers” [51]. Another factor that could increase demand for health services in general and hospital beds specifically is population growth and aging. Indeed, healthcare service utilisation among elderly populations aged 65 years and over, is higher in comparison to other age groups, showing both higher rates of admission and longer lengths of stay [44]. Therefore, in forecasting the future demand and planning for hospital expansion, this age group percentage must be taken into consideration.
The case of Kuwait
An overview of Kuwait’s national HCS: Broadly speaking, any HCS consists of the financer, the user and the provider. MOH is the main healthcare financier and provider in the state of Kuwait, while the private sector provides a small percentage of services. For example, the total number of beds in the private sector is 1082, while in MOH the total bed capacity is 7118 [52]. The MOH aims to distribute healthcare effectively, with high quality and productivity [53]. It is a non-profit organisation funded by the Kuwait government. The MOH is the responsible body for managing financial and human resources, the infrastructure, the facilities and the information systems. It also leads, organises, supervises and manages the activities of providing healthcare services, disease prevention and health promotion. Furthermore, it establishes the roles and regulations as well as developing and implementing the health plan and policies. All these activities are carried out and coordinated with the six regional health areas. Each health region area consists of a number of primary healthcare centres and one general hospital. The national statistical references are provided yearly by Kuwait’s MOH presented by the medical records department. In Table 2 an overview of development of medical staff/beds in Kuwait’s health sector is provided [54].
Table 2 Development of medical staff/beds in Kuwait’s health sector.
| Indicator | 1975 | 1985 | 1995 | 2000 | 2005 | 2010 | 2015 |
|---|---|---|---|---|---|---|---|
| Physicians | 932 | 2,528 | 2,788 | 3,204 | 4,150 | 5,680 | 8105 |
| Dentists | 85 | 277 | 409 | 517 | 679 | 1,123 | 1774 |
| Nurses | 3,660 | 8,187 | 7,618 | 8,232 | 9,419 | 15,283 | 21082 |
| Beds | 4,056 | 6,226 | 4,409 | 4,903 | 4,903 | 6,338 | 7,118 |
| Population per physician | 924 | 614 | 606 | 683 | 551 | 463 | 412 |
| Population per nurse | 246 | 189 | 222 | 266 | 273 | 202 | 153 |
| Population per bed | 241 | 294 | 383 | 479 | 520 | 485 | 496 |
| Physicians per bed | 0.2 | 0.5 | 0.6 | 0.8 | 1.0 | 1.0 | 1.1 |
| Nurses per bed | 1.0 | 1.6 | 1.7 | 1.8 | 1.9 | 2.4 | 2.9 |
In Kuwait, the expenditure in the healthcare services is increasing year after year and is expected to double within 5 years if we consider the statistics of the last 10 years (Table 3).
Table 3 Development of government expenditure on health care in Kuwait.
| Year | Total expenditure (Million KD) | Per capita expenditure (KD) | |||
|---|---|---|---|---|---|
| Nominal | Real | % of GDP | Nominal | Real | |
| 1970/1971 | 15.89 | 56.37 | 1.15 | 21.96 | 77.90 |
| 1974/1975 | 29.18 | 72.41 | 0.84 | 29.33 | 72.78 |
| 1979/1980 | 103.50 | 189.11 | 1.33 | 76.22 | 139.26 |
| 1984/1985 | 192.73 | 283.14 | 2.99 | 113.55 | 166.81 |
| 1989/1990 | 212.84 | 267.12 | 3.99 | 99.34 | 124.67 |
| 1994/1995 | 135.36 | 148.18 | 1.67 | 85.91 | 94.05 |
| 1999/2000 | 244.22 | 244.22 | 2.11 | 109.60 | 109.60 |
| 2004/2005 | 393.00 | 361.21 | 1.67 | 177.55 | 163.19 |
| 2008/2009 | 1,028.00 | 755.88 | 3.26 | 397.98 | 292.64 |
| 2014/2015 | 1,766.9 | 1,643.37 | 3.71 | - | 364 |
Note: Currently, 1 KD=3.3 US dollars.
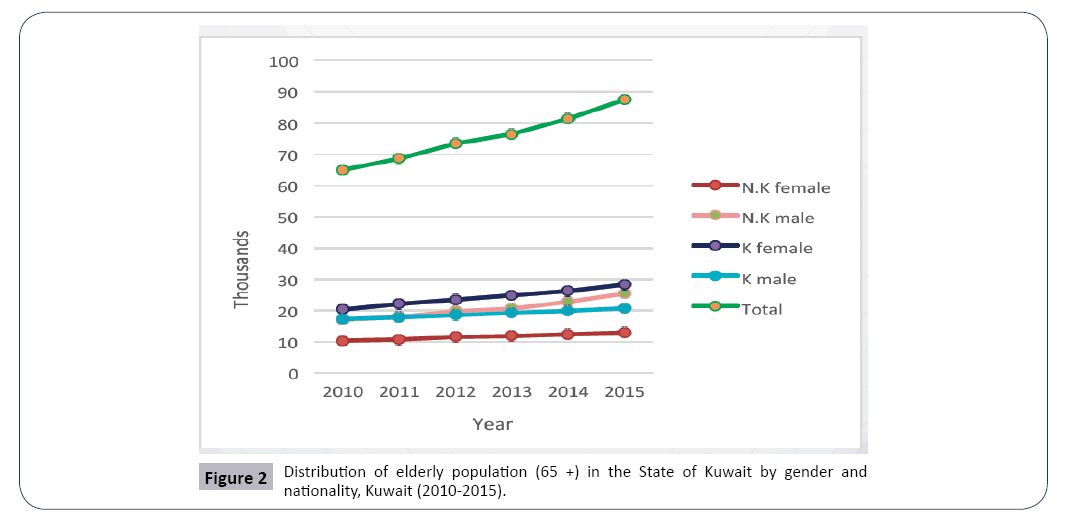
In 2005, a total of 361 million Kuwaiti Dinar (KD) was spent by the MOH, while in 2015 the number increased to 1,643, which accounts for 455% growth. Adding to that, the percentage of elderly people (>65 years) is growing (Table 4 and Figure 2).
Table 4 Distribution of Kuwait’s elderly population according to their gender and nationality.
| Years | Number and percentage | KUWAITI | Non-KUWAITI | Total | KUWAITI Population | Non-KUWAITI Population | KUWAITI Population | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Male | Female | % of elderly | Male | Female | % of elderly | Male | Female | % of elderly | |||||
| 2010 | n | 17246 | 20266 | 3.3 | 17087 | 10368 | 1.1 | 34333 | 30634 | 64967 | 113214 | 2433223 | 3566437 |
| % | 46 | 54 | 62.2 | 37.8 | 52.8 | 47.2 | 1.8 | ||||||
| 2011 | n | 17867 | 22097 | 3.4 | 17976 | 10708 | 1.2 | 35843 | 32805 | 68648 | 1164448 | 2467561 | 3632009 |
| % | 44.7 | 55.3 | 62.7 | 37.3 | 52.2 | 47.8 | 1.9 | ||||||
| 2012 | n | 18584 | 23490 | 3.5 | 19796 | 11596 | 1.2 | 38380 | 35086 | 73466 | 1195806 | 2610837 | 3806643 |
| % | 44.2 | 55.8 | 63.1 | 36.9 | 52.2 | 47.8 | 1.9 | ||||||
| 2013 | n | 19169 | 24864 | 3.6 | 20622 | 11826 | 1.2 | 39791 | 36690 | 76481 | 1227012 | 2664917 | 3891929 |
| % | 43.5 | 56.5 | 63.6 | 36.4 | 52 | 48 | 2 | ||||||
| 2014 | n | 19895 | 26269 | 3.7 | 22769 | 12427 | 1.3 | 42664 | 38696 | 81360 | 1258254 | 2781191 | 4039445 |
| % | 43.1 | 56.9 | 64.7 | 35.3 | 52.4 | 47.6 | 2 | ||||||
| 2015 | n | 20737 | 28321 | 3.8 | 25401 | 12893 | 1.3 | 46138 | 41214 | 87352 | 1291401 | 2892257 | 4183658 |
| % | 42.3 | 57.7 | 66.3 | 33.7 | 52.8 | 47.2 | 2.1 | ||||||
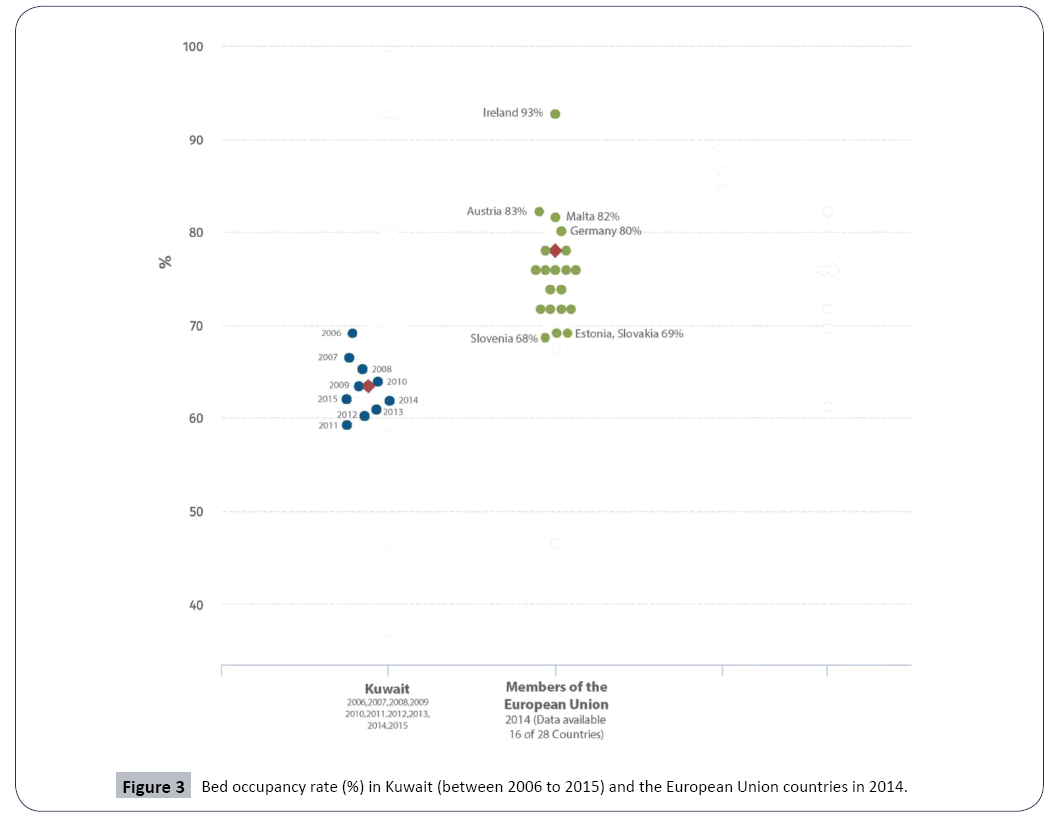
There was a steady increase in the percentage of the elderly from 2010 to 2015 among the total population in Kuwait, reaching 3.8% in 2015 [55]. Kuwait’s MOH should consider all the previous data for the future planning especially for the decision of adding more beds. Occupancy rate between Kuwait and Europe: In Kuwait, hospital bed capacity is determined by the MOH. The approach to determine hospital bed capacity is not very clear. Indeed, both the national level ratio of beds for 100,000 inhabitants in each category and the target bed occupation is a common method used to define hospital bed capacity. A 100% bed occupancy rate will hardly ever be reached. Different countries had different bed occupancy rates where they have a variety of institutional settings. A comparison between the bed occupancy rate (%) in Kuwait (2006 to 2015) and the European Union countries in (2014) can be illustrated in Figure 3.
In European Union countries, a significant difference is found in bed occupancy rates. Based on the WHO’s most recent statistics in 2014, the average occupancy rate of Europe Union countries is 77% [56]. Ireland had the highest bed occupancy rate with 93% of beds, while Slovenia had the lowest rate, at about 68% [56]. On the other hand, in the last ten years, the bed occupancy rate in all Kuwait government hospitals did not exceed 69.3% with an average of 63.6% between the period from 2006 to 2015 (Table 5).
Table 5 Bed utilisation indices in M.O.H. hospitals, Kuwait 2006-2015.
| Utilisation Indices | 2006 | 2007 | 2008 | 2009 | 2010 | 2011 | 2012 | 2013 | 2014 | 2015 | |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Bed occupancy rate | 69.3 | 66.7 | 65.7 | 63.3 | 64.8 | 59.4 | 60.4 | 61.1 | 62.1 | 63.3 | |
| Average length of stay* | 5.5 | 5.6 | 5.8 | 5.7 | 5.9 | 5.7 | 6 | 6 | 6.2 | 6.2 | |
| Bed complement | 5149 | 5424 | 5614 | 6072 | 6338 | 6703 | 6714 | 6851 | 6962 | 7118 | |
*Excluding Psychological Medicine Hospital and Physical Medicine and Rehabilitation Hospital
It is worth noting that the incapability of the healthcare decision makers to handle hospital operations efficiently in an integrative way will make the case more complicated resulting in wasting costly resources, inefficient bed utilisation and poor patient flow. This could be exemplified by an overcrowded emergency department, patient misplacements, surgery cancellations and long waiting lists, which could directly influence the healthcare service quality. Consequently, it is crucial to utilise hospital resource efficiency. In the HCS, the inevitable variability will affect both the quality of the healthcare service levels and the resource utilisation [10,39,40]. The fluctuation of bed capacity requirements is mostly due to the variable patient lengths of stay and the unpredictable patient demand [57]. Even with the low hospital bed occupancy rate in comparison to European countries, Kuwait’s government has taken the decision to expand their bed capacity in the next few years.
Hospital bed expansion: Kuwait’s HCS is currently facing many unprecedented challenges and potential changes. Kuwait’s government has been constantly vigilant about their HCS, attempting to improve their service efficiency and effectiveness. The Kuwaiti government has made extensive investments in healthcare infrastructure by building hospitals and clinics. The Kuwaiti MOH is currently undergoing a structural change in terms of total bed capacity. Currently 10 mega projects worth approximately 2 billion KD are being constructed in Kuwait [16]. The number of beds per thousand population increased from 1.8 in 2007 to 2.1 in 2013 [53]. Even more, in comparison to 2013 where the total bed capacity of the governmental sector was 6663, the number of beds is expected to reach 13474 in 2020. This means that the bed capacity is expected to be doubled by adding 6772 beds. This decision is considered a big challenge especially with 63.6% average occupancy rate between the period from 2006 to 2015
The needed bed capacity, their geographical distribution and guided policy for admission are related to the regional or national plans not at a hospital level. Therefore, before taking any action, it is necessary that the public authority review their existing situation regarding the previous factors. Furthermore, it is crucial to assess the economic cost of adding more beds to the existing capacity and understand how costly it is to maintain excess capacity. The national health organizational is a body required to assess the bed allocation and also the usage rules. Bed allocation “means assigning beds to various patient categories according to medical specialty, accommodation type, and logistical considerations; presumably, patient needs, research goals, and educational requirements are taken into account, along with cost” [51]. Healthcare policy makers must take into consideration the effects of their expansion decisions in the bed capacity. Sometimes bed expansion is not a solution for busy emergency departments or other specialties such as medical wards or intensive care units. However, running the hospital efficiently, reallocating the bed distribution and proper bed utilisation go some way to solving a busy hospital and providing the services for the patient when they are needed. In addition, there is a necessity to improve the approach of providing the services for the patients and running the Kuwait HCS in more efficient ways which could be by adopting lean.
Lean and hospital bed utilization: One way to lower the bed cost is to improve and enhance their utilisation [7]. A study [14] identified three strategies for efficient utilisation of hospital bed capacity, which are increasing occupancy rates, reducing the average LOS (by either discharging patients at an earlier stage of recovery or making use of new technologies) and/or decreasing admissions. Lean could be the method for achieving the previous three strategies. Lean was introduced as a management philosophy and improvement approach across many countries worldwide [58]. Lean (born in the industrial sector) promises to provide more with less. Four common themes were identified from lean philosophy: process-based view, eliminating waste, focus on value, and employee-driven change [59]. Lean aims to provide value to the patient by eliminating waste from the processes, which is usually presented by time spent waiting between and for services [60]. If the waste is removed from the care processes, patients will flow smoothly and continuously without interruption and with minimum waiting resulting in improving resources utilisation, service efficiency and patient care generally [61]. Therefore, lean philosophy could have an essential role in enhancing the utilisation of the existing beds capacity and planning for any future requirements. An example of that, a delay associated with the discharge process of a patient who is ready for discharge leads to occupying a bed unnecessarily. Therefore, inappropriate usage of the existing beds is considered as a main factor that affects their efficiency. Lean works by considering the hospital as a production system, where the different existing resources are directed to support the patient flow. This production system is open to the patients with different needs, time patterns and complaints, which are considered as the demand. On the other hand, the hospital supply consists of human resources (e.g. surgeons, nursing, administration staff) and the material resources (e.g. operating rooms, beds, machines, medicines). Therefore, the hospital is required to balance between the supply and demand in the best possible way, to achieve an efficient productive system. Indeed, the harmony in utilising hospital beds resulted in a well-organized effective patient flow in the HCS [57].
Conclusion
It is time to raise the following question: is there a requirement to add excess capacity in Kuwait’s healthcare organization? And if so, from economic analysis, what is the cost of that excess capacity and how will it be reflected on the quality of services. The decision of expanding an organisation’s bed capacity and infrastructure required bringing together all key stockholders under one umbrella and adopting analytical strategies that helps in making the right decisions considering the allocation and use of the existing hospital beds and added extra beds where it is required in order to have an efficient service. This paper highlights lean as an approach of optimising the use of the existing resources and managing the bed occupancy in an efficient way. In addition, the article explores the different factors that affect the decision of expanding the organization’s bed capacity and the influence of empty beds. Our discussion has at least one vital implication for public policy by reading the previous 10 years data of the bed occupancy rate. Kuwait’s MOH requires more in-depth studying for the idea of adding more beds with examining the implications on different aspects. Policy makers are required to have a sustainable system and balancing between the needs and demands. Different organizations in different countries are alert of the necessity to utilise their resources, especially the beds as efficiently as possible, particularly with the financial pressures. At the same time, it is essential to grant that the patient receives the appropriate healthcare services in the time they need it. It is worth noting that, it is inadequate only using and targeting the bed occupancy levels as the primary determinant of bed capacity [20]. However, managing bed capacity efficiently must consider the complexities of healthcare sectors in terms of trade-offs between demands from competing sources and types of patients, bed flexibility and quality of care, time-varying demands, and the habitually opposing perspectives of physicians, administrators, nurses and patients [10]. In order to understand the impact and relations between bed capacity and patient service, more sophisticated approaches are required to support decision making.
Future research
To advance our understanding for the optimal bed occupancy rate in the 21st century more research is needed considering the different variability on the level of the hospital, the organization, on regional, national and international level. Therefore, more research should be carried out at micro, meso and macro levels. Furthermore, for any organization stepping forward to expand their infrastructure and bed capacity, an evaluation of the effects of these changes should be studied, investigated and calculated. Another direction of research is to study lean as an approach for improving the efficiency of bed utilisation as specific and as a management approach for improving the patient flow in general.
The following are some of the questions that should be raised in case the national organization is looking in future to increasing their bed flexibility, increasing the efficiency and service performance and developing a regional capacity planning:
• “What are the optimal policies for opening and shutting a normally unused overflow unit?
• How many swing beds should a hospital have and for which clinical services?
• How should clinical units be used to “back up” each other so as to minimize overall off-service placements without jeopardizing the timely provision of care?
• How should outpatient (or elective patient) schedules be designed so as to allow for timely access by emergency patients and/or inpatients without resulting in unacceptable backups?
• Given the costs of delay for each patient type, what dynamic priority rules are optimal for allocating time slots during the day when more than one type of patient is waiting?
• Assuming that the likelihood of cancellations and “noshows” increases with the duration of time between when an appointment is made and the scheduled examination date, what is the optimal length of the scheduling horizon?
• When a hospital has multiple diagnostic or treatment facilities, how many and which patient categories should be assigned to each?
• How should hospital planning regions be defined? Should this definition differ by clinical service?
• When should a hospital go on ambulance diversion? How should this be affected by conditions at the other hospitals in the region?
• How should a hospital’s “surge capacity” (the percentage increase in demand above normal levels that can be “adequately” accommodated), be defined and predicted?”
Limitation
This study has some limitations. The first one is related to the secondary health data acquired from Kuwait’s MOH annual records. These routinely collected data are general, unspecific and were not collected for the purpose of this article. Besides which, it is the only available data source. However, the drawn conclusion, building on these data, is worthwhile as the aim of this paper is to highlight the importance of the way decisions are made for the organisation to expand and not to study the current situation in-depth. The other limitation is using the developed countries’ data that could have a different context and healthcare settings. This could make the comparison unspecific. Indeed, many of the developed countries, for example the UK, have a similar system to Kuwait. Finally, other factors should be considered including the private healthcare sector, the medical insurance companies and treatment obtained overseas.
Ethics
The study was based on using the routinely collected data from Kuwait’s MOH, that are published publicly and can be accessed online. Therefore, no ethics approval was necessary.
References
- Duran A, Dubois HF, Saltman RB (2011) The evolving roles of hospitals and recent concepts of public sector governance. Governing Public Hospitals: Recent Strategies and the Movement toward Institutional Autonomy. Brussels: Eur Observatory Sys and Policies 15-34.
- Hershey JC, Weiss EN, Cohen MA (1981) A stochastic service network model with application to hospital facilities. Operations Res 29: 1-22.
- Dumas MB (1984) Simulation modeling for hospital bed planning. Simulation 43: 69-78.
- Vassilacopoulos GA (1985) Simulation model for bed allocation to hospital inpatient departments. Simulation 45: 233-241.
- Worthington D (1987) Queueing models for hospital waiting lists. J Opt Res Soc 38: 413-422.
- Schwartz WB, Joskow PL (1980) Duplicated hospital facilities: How much can we save by consolidating them? New Eng J Med 303: 1449-1457.
- Keeler TE,Ying JS (1996) Hospital costs and excess bed capacity: A statistical analysis. The Review Eco Sta 78: 470-481.
- Gaynor M, Anderson GF (1995) Uncertain Demand. The Structure of Hospital Costs, and the Cost of Empty Hospital Beds. J Health Eco 14: 291-317
- Pauly MV, Wilson P (1986) Hospital output forecasts and the cost of empty hospital beds, Health Services Res 21: 403-428.
- Green LV (2005) Capacity planning and management in hospitals. Operations Res Health Care 70: 15-41.
- Abdelaziz B, Masmoudi FM (2012) A multiobjective stochastic program for hospital bed planning. J Oper Res Soc. 63: 530-538.
- Vetter N (2003) Inappropriately delayed discharge from hospital: What do we know? British Medi J 326: 927-928.
- Glasby J, Littlechild R, Pryce K (2006) All dressed up but nowhere to go? Delayed hospital discharges and older people. J Heal Ser Res & Poli 11: 52-58.
- Kroneman M, Siegers JJ (2004) The effect of hospital bed reduction on the use of beds: A comparative study of 10 European countries. Social Sci Medi 59: 1731-1740.
- Saltman RB, Figueras J (1998) Analyzing The Evidence On European Health Care Reforms: Experience in western European health care systems suggests lessons for reform in the United States, according to a major international comparison by the World Health Organization. Health Affairs 17: 85-108.
- Kelendar H, McIntosh B (2017) Exporting the NHS: The near future. British J Health Care Man 23: 6-7.
- Ahmed JU (2010) Documentary research method: New dimensions. Indus J Man & Social Sci 4: 1-14.
- Bailey KD (1994) Methods in social research. (4thedn), New York, The Free Press.
- Judd CM, Smith ER, Kidder LH (1991) Research methods in social relations. trove National lib of Australia.
- Green LV, Nguyen V (2001) Strategies for cutting hospital beds: The impact on patient service. Health Serv Res 36: 421-442.
- OECD, Health at a Glance 2017. 2017.
- NHS. E ( 2017) Bed availability and occupancy, 7 June 2019.
- FA Sloan, Valvona J (1986) Why has hospital length of stay declined? An evaluation of alternative theories. Soc Sci Med 22: 63-73.
- Smet M (2007) Measuring performance in the presence of stochastic demand for hospital services: An analysis of Belgian general care hospitals. J Prod Anal 27: 13-29.
- Duncan GM (1990) The effect of probabilistic demands on the structure of cost functions. J Risk and Uncertainty 3: 211-220.
- Roemer MI (1961) Bed supply and hospital utilization: A natural experiment. Hospitals 35: 36-42.
- Brecher C (1995) Privatization and public hospitals: Choosing wisely for New York City. Brookings Inst Press, Washington, DC, 99.
- Toussaint E (2001) Method to determine the bed capacity, different approaches used for the establishment planning project in the University Hospital of Nancy. Study health Tech Info 8: 1404-1408.
- NguyenJM, Six P, Antonioli D, Glemain P, Potel G, et al. (2005) A simple method to optimize hospital beds capacity. Int J Med Inform.74: 39-49.
- Kuntz L, Scholtes S,Vera A (2007) Incorporating efficiency in hospital-capacity planning in Germany. Eur J Health Econ 8: 213-223.
- Clerkin D, Fos PJ, Petry FE (1995) A decision support system for hospital bed alignment. Hospital Health Serv Adm 40: 386-400.
- Lyons RA, Wareham K, Hutchings HA, Major E, Ferguson B (2000) Population requirement for adult critical-care beds: A prospective quantitative and qualitative study. The Lancet 355: 595-598.
- Jung AL, Streeter NS (1985) Total population estimate of newborn special-care bed needs. Pediatrics 75: 993-996.
- Plati C, Lemonidou C, Priami M, Baltopoulos G, Mantas J (1996) The intensive care units in greater Athens: Needs and resources. Int Crit Care Nurse 12: 340-345.
- Jill P, David F, Janet R, Philip S (2000) National census of availability of neonatal intensive care. BMJ 321: 727-729.
- Lampl C, Klingler D, Deisenhammer E, Hagenbichler E, Neuner L, et al. (2001) Hospitalization of patients with neurological disorders and estimation of the need of beds and of the related costs in Austria’s non-profit hospitals. Eur J Neurol. 8: 701-706.
- Baker LC, Ciaran SP, Cassandra G, Dylan S, James LR (2004) Within-year variation in hospital utilization and its implications for hospital costs. J Health Econ. 23: 191-211.
- VanBerkel PT, Blake JT (2007) A comprehensive simulation for wait time reduction and capacity planning applied in general surgery. Health Care Man Sci 10: 373-385.
- Harper PR, Shahani A (2002) Modelling for the planning and management of bed capacities in hospitals. J Operat Res Society 53: 11-18.
- Ma G, Demeulemeester E (2010) Assessing the performance of hospital capacity planning through simulation analysis.
- Adan I, Jos B, Nico D, Jully J, Jan V (2011) Improving operational effectiveness of tactical master plans for emergency and elective patients under stochastic demand and capacitated resources. Eur J Oper Res 213: 290-308.
- Li LX, Benton WC, Leong GK (2002) The impact of strategic operations management decisions on community hospital performance. J Oper Manag 20: 389-408.
- Brailsford SC (2007) Advances and challenges in healthcare simulation modeling: Tutorial. IEEE Press 1436-1448.
- Seematter BL, Fustinoni S, Dung DH, Eggimann BS, V Koehnc, et al. (2015) Comparison of different methods to forecast hospital bed needs. Euro Geriatric Medi 6: 262-266.
- Litvak E, Long MC (2000) Cost and quality under managed care: Irreconcilable differences. American J Man Care 6: 305-312.
- Burns LR, Andersen RM, Shortell SM (1989) The impact of corporate structure on physician inclusion and participation. Medical Care 27: 967-982.
- Boutsioli Z (2010) Demand variability, demand uncertainty and hospital costs: A selective survey of the empirical literature. Global J Health Sci 2: 138.
- Lynk WJ (1995) The creation of economic efficiencies in hospital mergers. J Health Economics 14: 507-530.
- Gorunescu F, McClean SI, Millard PH (2002) A queueing model for bed-occupancy management and planning of hospitals. J Operational Res Society 53: 19-24.
- Almeida AS, Cima JF (2015) Demand uncertainty and hospital costs: An application to Portuguese public hospitals. Eur J Health Econ 16: 35-45.
- Dumas MB (1985) Hospital bed utilization: An implemented simulation approach to adjusting and maintaining appropriate levels. Health Services Res 20: 43.
- Kuwait Ministry of Health, Annual Health Report (2015) National Center of Health Information, Ministry of Health: Kuwait.
- Kuwait Ministry of Health (2013), World Health Survey in Kuwait.
- Central-Statistical-Bureau, Annual Statistical (2016) Kuwait.
- Kuwait Ministry of Health, Health Profile of the Elderly in Kuwait (2016) Key Indicators, t.G.H.S. Administration, Editor, Kuwait MOH: Kuwait.
- WHO Regional Office for Europe. European Health Information Gateway: Bed occupancy rate (%) (2014).
- Ma G, Demeulemeester E (2013) A multilevel integrative approach to hospital case mix and capacity planning. Comp Operations Res 40: 2198-2207.
- Mazzocato P, Savage C, Brommels M, Aronsson H, Thor J (2010) Lean thinking in healthcare: A realist review of the literature. Qual Saf Health Care 19: 376-382.
- Radnor Z, Walley P (2008) Learning to walk before we try to run: adapting lean for the public sector. Public Money Man 28: 13-20.
- Khan NS, Jain S (2010) Quality initiatives in the emergency department. Current Opinion Pedia 22: 262-267.
- Holden RJ (2011) Lean Thinking in emergency departments: A critical review. Ann Emerg Med 57: 265-278.
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences