How should Masih Daneshvari Hospital in Tehran Prepare for Coronavirus Disease 2019?
Beheshteh Jebelli, Mohammad Varahram, Masoud Soltanifard Razlighi, Mojgan Palizdar, Elham Ghazanchaei
DOI10.36648/2471-9781.20.6.254
1Clinical Tuberculosis and Epidemiology Research Center, National Research Institute of Tuberculosis and Lung Diseases (NRITLD), Shahid Beheshti University of Medical Sciences, Tehran, Iran
2Mycobacteriology Research Center, National Research Institute of Tuberculosis and Lung Diseases (NRITLD), Shahid Beheshti University of Medical Sciences, Tehran, Iran
3Director Administrative Affairs Masih Daneshvari Hospital, Tehran, Iran
4Infection Control Supervisor Masih Daneshvari Hospital, Tehran, Iran
5Chronic Respiratory Diseases Research Center, National Research Institute of Tuberculosis and Lung Diseases (NRITLD), Shahid Beheshti University of Medical Sciences, Tehran, Iran
- *Corresponding Author:
- Elham Ghazanchaei
Chronic Respiratory Diseases Research Center
National Research Institute of Tuberculosis and Lung Diseases (NRITLD)
Shahid Beheshti University of Medical Sciences, Tehran, Iran
E-mail: El_gh2008@yahoo.com
Received Date: May 25, 2020; Accepted Date: June 09, 2020; Published Date: June 24, 2020
Citation: Beheshteh J, Mohammad V, Masoud SR, Mojgan P, Elham G (2020) How should Masih Daneshvari Hospital in Tehran Prepare for Coronavirus Disease 2019? J Hospital Med Mang. Vol. 6 No. 3: 254.
DOI: 10.36648/2471-9781.6.3.254
Abstract
In the first days of the year 2020, there was a report of an outbreak of Coronavirus respiratory tract infectious disease in Wuhan, China [1]. Coronavirus is a pathogen able to be transmitted from animals to human and spread from human to human [2]. This disease called COVID-19 is known as SARS-COV2, the complete genome sequence of which is screened by Polymerase Chain Reaction (PCR) analysis and patients’ tracheal secretion culture [3,4]. The genome of this virus as the seventh coronavirus that infects human, is similar %80 to Severe Acute Respiratory Syndrome Coronavirus (SARS-COV), %50 to Middle East Respiratory Syndrome Coronavirus (MERS-COV), and %96 to Bat Coronavirus, and utilizes a cell receptor, Angiotensin-Converting Enzyme II (ACE2), also used by SARS [5]. Wuhan was put under quarantine on January 23, 2020 [6]. In mid-January, over 2800 positive cases were reported in China [7]. The first confirmed death from coronavirus infection was reported on January 9 [8]. On January 30 2020, WHO released a statement declaring the outbreak of novel coronavirus as a global health emergency [9] and on March 11 2020, it was declared a pandemic [10]. Coronavirus was officially declared to have entered Qom, Iran on February 18 2020 [11]. At that time, 27 hospitals across the country announced their readiness as referral hospitals to admit and care for patients with coronavirus, and Masih Daneshvari Hospital in Tehran was among the first hospitals that held its first emergency meeting immediately after its readiness announcement to the Ministry of Health and Medical Education of Iran on February 20, 2020, to provide effective strategies for the prevention of COVID-19 transmission in healthcare settings and for the referral and patient management.
Introduction
In the first days of the year 2020, there was a report of an outbreak of Coronavirus respiratory tract infectious disease in Wuhan, China [1]. Coronavirus is a pathogen able to be transmitted from animals to human and spread from human to human [2]. This disease called COVID-19 is known as SARSCOV2, the complete genome sequence of which is screened by Polymerase Chain Reaction (PCR) analysis and patients’ tracheal secretion culture [3,4]. The genome of this virus as the seventh coronavirus that infects human, is similar 80% to Severe Acute Respiratory Syndrome Coronavirus (SARS-COV), 50% to Middle East Respiratory Syndrome Coronavirus (MERS-COV), and 96% to Bat Coronavirus, and utilizes a cell receptor, Angiotensin- Converting Enzyme II (ACE2), also used by SARS [5]. Wuhan was put under quarantine on January 23, 2020 [6]. In mid-January, over 2800 positive cases were reported in China [7]. The first confirmed death from coronavirus infection was reported on January 9 [8]. On January 30 2020, WHO released a statement declaring the outbreak of novel coronavirus as a global health emergency [9] and on March 11 2020, it was declared a pandemic [10]. Coronavirus was officially declared to have entered Qom, Iran on February 18 2020 [11]. At that time, 27 hospitals across the country announced their readiness as referral hospitals to admit and care for patients with coronavirus, and Masih Daneshvari Hospital in Tehran was among the first hospitals that held its first emergency meeting immediately after its readiness announcement to the Ministry of Health and Medical Education of Iran on February 20, 2020, to provide effective strategies for the prevention of COVID-19 transmission in healthcare settings and for the referral and patient management.
Quality Improvement Management and Disaster Preparedness and Response
The most basic action was to evacuate the hospital of already hospitalized patients and to prepare wards for the admission of COVID-19 patients and to shut down clinics. As shown in (Table 1)
Table 1 Setting Up Isolation Wards in Masih Daneshvari Hospital for Admission of COVID-19 Patients.
| Phase | Wards | No. of Beds | Operation Date dd/mm/yyyy | Operation Status | |
|---|---|---|---|---|---|
| First | ICU - Acute Respiratory Diseases | 7 | 20/02/2020 (Morning) | Hospitalization | |
| Infectious Diseases Department 5 | 24 | 20/02/2020 (Morning) | Hospitalization | ||
| Second | Infectious Disease-Related Emergency | 8 | 20/02/2020 (Afternoon) | Hospitalization | |
| Internal 3 | 31 | 20/02/2020 (Afternoon) | Hospitalization | ||
| Third | Internal 4 | 31 | 22/02/2020 | Hospitalized | |
| Fourth | Thoracic Surgery | 33 | 23/02/2020 | Prepared for Admission | |
| ICU – Surgery | 13 | 23/02/2020 | Prepared for Admission | ||
| Fifth | Oncology | 19 | 25/02/2020 | Preparing | |
| ICU – Emergency | 7 | 25/02/2020 | Preparing | ||
| Sixth | ICU – Internal | 7 | 29/02/2020 | Preparing | |
| ENT Surgery | 12 | 29/02/2020 | Preparing | ||
| Seventh | Internal 9 | 25 | 01/03/2020 | Preparing | |
| ICU – Infectious Disease-Related Emergency | 2 | 01/03/2020 | Preparing | ||
| Eighth | Post Angiography | 14 | 02/03/2020 | Preparing | |
| Ninth | Setting Up Eight ICU Beds in ENT Surgery Department Setting Up Eight ICU Beds in Infectious Diseases Department 5 Setting Up Twenty ICU Beds in Internal Department 4 |
Four Days After the Supply of Special Equipment | |||
| Tenth | Implant Department (Development) | 32 Special-purpose Beds | Four Days After the Supply of Special-purpose Equipment | ||
All and any communicated directives and circulars of the Ministry of Health and Medical Education were received and the Office for Quality Improvement was held responsible to monitor their proper implementation and execution.
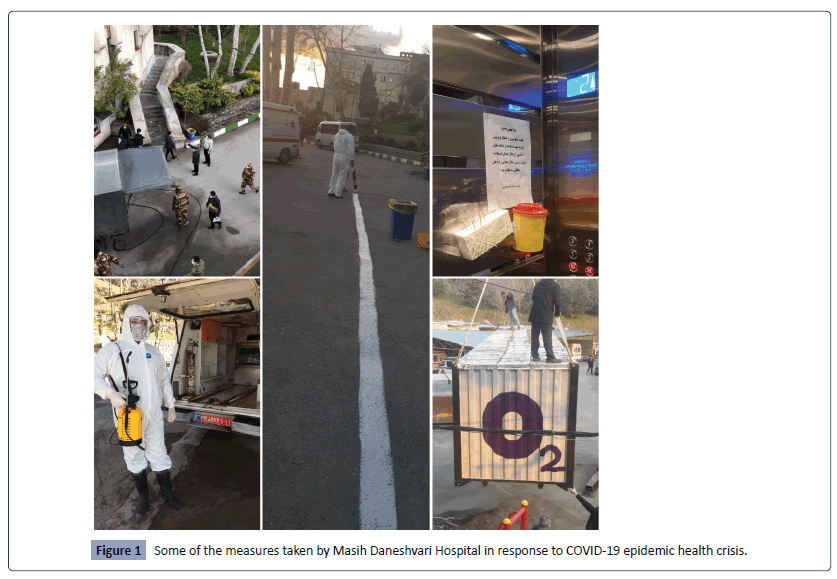
The next step was medical and office support staff management in the form of calling for retired medical workers and those on leave and giving leave to high-risk employees (i.e. Pregnant employees, those suffering from immunodeficiency disorders, those taking corticosteroids and immunosuppressive drugs). Non-attendance of administrative research staff, attendance of 1/3 of administrative non-research staff and related decisions are made by the relevant authority based on the administration type and nature as well as the workload. Medical learners, nursing and other paramedical students have been prohibited from entering the premises to reduce the traffic flow in wards and bedside visits. The CPR team of the hospital is minimized to the least possible number of members, including an anesthesiologist, a nurse, a technician and a physician in attendance, for traffic flow management and less physical contacts. Also organizing outstation volunteers are made through their admission in different hospital departments including medical wards, catering, mortuary, infection control and environmental health division, laboratories and other divisions, based on the urgent needs and specialty of each person. Before starting their work, each volunteer goes under health check and parasite test, and their body temperature and exposure history are taken, etc. Military forces have been responsible for the weekly disinfection of the entire premises and medical and Para clinical wards of the hospital utilizing full equipment. In the telenursing system, 3 nurses are responsible in a full-time basis to train patients discharged from the hospital and those in quarantine. This has prevented unnecessary referral of about 600 patients to hospital Emergency department and their hospitalization for 2 months. In phone interviews with patients, 5 areas including nutrition, physical activity, sleep quality, quarantine principles and health promotion are reviewed and trained. Besides, follow-up after discharge is being performed in another department by SMSs and through the application designed for this purpose. In such system, there is a two-way interactive text messaging on patients’ after-discharge condition and homecare training tips are sent daily in a training application (Figure 1).
In the part of hospital equipment development and efficiency, twofold commissioning of hospital medical waste disposal system was done in consideration of the increase in the infectious waste generation in the early days. Two oxygen concentrators using bank-type technology with 1000 liter/minute capacity are installed to support the needs of respiratory patients. Also, one oxygen concentrator with 500 liter/minute capacity is installed in the hospital new Emergency building. Two ECMO machines as temporary replacement for patients’ damaged heart and lungs are purchased and entered the treatment cycle to be used for patients with indications. Also, a portable digital X-ray machine for the respiratory intensive care unit is prepared to reduce traffic flow in the premises.
In a few weeks from the COVID-19 epidemic in Iran, the Plasma donation unit collaborated by Iranian Blood Transfusion Organization and the Ministry of Health and Medical Education is operating for the treatment of COVID-19 patients.
Infection Control
Patients enter the hospital from the pre-determined route towards the infectious disease-related emergency department. Waiting area is outdoor in a large space to make it possible to distance between clients who have received the queue number. Fast acting disinfectant spray is used to disinfect surfaces touched by clients including chairs. Pulse oximetry sensor surface is disinfected with sterile alcohol wipes after each single use for patients. Medical masks are available for all suspicious and infected clients to prevent their flow in the hospital without masks. 3 hospital staff are responsible in every work shift to carry out the admission and hospitalization process in the department for absolute prevention of patient flow in hospital premises. Disinfectant dispensers are mounted next to personnel attendance machines and the personnel entry and exit is controlled visually as much as possible. In the place of high-touch surfaces such as elevator buttons, toothpicks and safety boxes are placed to prevent surface touch as much as possible.
The infectious disease-related emergency department decides whether the patient has to be hospitalized or placed in quarantine. Upon receiving the travel history or contacts data and after examinations, patients with shortness of breath, fever, cough and O2sat drop to under 93% are candidates for hospital admission. Throat swab culture is done at the beginning of patient hospitalization and lung CT scanning is considered as the most basic and accurate method providing definitive diagnosis. Visiting patients is totally forbidden and patients’ spiritual and psychological need to have contacts with their families is met through phone and visual contracts by cellphones and tablets. All patients’ paper and semi-paper-based records are transformed to fully electronic records so to prevent an inter-ward paper transfer and infection agents transfer as much as possible. Ambulances are entirely disinfected every day after patient transfers and personnel transportation services. At the time of a patient’s death, the attendance of his/her companions is managed in the form of their direct referral to the admitting department and receiving relevant hospital papers. Companions may not mourn in the mortuary. Based on the approval of the Infection Control Committee, all high-risk surfaces such as nurses stations, keys and door handles are disinfected every 4 hours. Close suction is used in intensive care units to discharge secretions and prevent the virus from spreading as much as possible.
The 6-course protein-vitamin rich diet for patients and staff has been among other measures taken to strengthen their immune system. In line with strengthening staff’s immune system, there has been a multivitamin injection vial infusion for each one of them. Also, all the staff has undergone Immune Assessment Test. Rooms to change gowns are determined in every department to prevent the infection spread at the time of dress changing. Nevertheless, it is about 64 out of 1100 (5-8%) personnel of Masih Daneshvari Hospital who have caught coronavirus when dealing with patients, fortunately none has died and they have gone through the disease process with different clinical manifestations from mild to acute.
Despite all protective measures, the coronavirus spread is unbelievably rapid and based on various reports from around the world it seems that diverse clinical manifestations have remained this type of coronavirus unknown. The lack of timely identification of this virus may paralyze a hospital and incur heavy losses [12]. Considering the unknown Nature and behavior of COVID-19 virus in different conditions, sharing experiences by world health centers may contribute to the process of identification and control of the COVID-19 global epidemic.
References
- Hoe G W, Wah L J, KOH D (2020) Preventing intra-hospital infection and transmission of COVID-19 in healthcare workers.
- Bhagavathula AS, Aldhaleei WF, Rahmani J, Ashrafi MM, Kumar BD (2020) Novel Coronavirus (COVID-19) Knowledge and Perceptions: A Survey of Healthcare Workers.
- Zhu N, Zhang D, Wang W, Li X, Yang B, et al. (2020) A novel coronavirus from patients with pneumonia in China, 2019. N Engl J Med 382:727-733.
- Zhou P, Yang XL, Wang XG, Hu B, Zhang L, et al. (2020) A pneumonia outbreak associated with a new coronavirus of probable bat origin, Nature.
- M. Arabi Y, Murthy S, Webb S (2020) COVID-19: a novel coronavirus and a novel challenge for critical care. Intensive Care Med.
- Hui, Jane Li, Mary. "China has locked down Wuhan, the epicenter of the coronavirus outbreak". Quartz. Retrieved 23 January 2020.
- Field (2020)."Nine dead as Chinese coronavirus spreads, despite efforts to contain it". The Washington Post. Retrieved 22 January 2020.
- Qin Amy, Hernández, Javier C (2020) "China Reports First Death from New Virus". The New York Times. Archived from the original on 11 January 2020.
- World Health Organization. Statement on the second meeting of the International Health
Regulations (2005) Emergency Committee regarding the outbreak of novel coronavirus. - World Health Organization. WHO Director-General’s opening remarks at the media briefing on COVID-19 – 11 March 2020.
- Official statistics of people with coronavirus in Iran. "Official statistics of people with coronavirus in Iran. 2020-03-14. Retrieved 2020-03-14.
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences