It is Time for More Physician and Nursing Representation on Hospital Boards in the US
Bhagwan Satiani and Suraj Prakash
DOI10.4172/2471-9781.100011
Bhagwan Satiani* and Suraj Prakash
The Ohio State University College of Medicine, USA
- Corresponding Author:
- Bhagwan Satiani
Professor Clinical Surgery,
The Ohio State University College of Medicine
St# 700; 376 W. 10th Avenue, Columbus, OH 43210, USA
Tel: 614-293-8536
Fax: 614-293-8902
Received Date: May 11, 2016; Accepted Date: June 22, 2016; Published Date: June 27, 2016
Citation: Satiani B, Prakash S. It is Time for More Physician and Nursing Representation on Hospital Boards in the US. J Hosp Med Manage. 2016, 1:2.
Abstract
Members of hospital boards are fiduciaries with a legal responsibility to fulfilling the hospital’s mission. Members represent a variety of community members and are responsible for ensuring patient safety and quality of care as well as evaluating the chief executive. Clinicians serve on the board but their numbers are limited and generally under 20%. We review the current state of hospital boards and suggest that physicians, nurses and other clinicians contribute considerably to expertise related to patient safety and more of them should be appointed to hospital boards
Introduction
According to the American Hospital Association, there are currently 5,627 registered hospitals in the US, of which 87.5% are community hospitals [1]. Among community hospitals, 58% are nongovernment owned not-for-profit (NFP), 20% are state and local government funded and 19% are investor-owned for-profit. Federal government hospitals comprise 7.2% of all registered hospitals. The remaining hospitals are nonfederal psychiatric hospitals, nonfederal long term care hospitals and hospital units of institutions (i.e. prison hospitals, college infirmaries, etc.).
Hospital boards are governing bodies that serve in both an advisory and oversight capacity in the interest of a hospital’s owners, which in all NFP’s are local communities. In for–profit hospitals, most owners are shareholders or private owners. By design, boards are intended to act as independent agents of the hospital as an intermediary between executive management and hospital ownership. Ownership of hospitals across the US varies greatly and includes public ownership (i.e. through publicly traded stocks), private ownership and government ownership. The specific structure, membership and duties of boards are dictated by the organization’s bylaws..
Board Composition and Responsibilities
The senior author has served on a large NFP health system board for several years. In addition, a google search was conducted using words like: hospital board, hospital board trustee, physician board members, nursing hospital board members and hospital board compensation.
Hospital boards are generally made up of representatives from the local community such as business leaders, lawyers, government and private sector leaders, physicians, nurses and others [2]. Medical staff and the board have different roles and responsibilities in a hospital. The medical staff’s primary role is to oversee quality, patient safety and physician credentialing. Typical responsibilities of hospital boards include the establishment of a broad organization strategy, financial resource allocation, internal auditing, risk management, future board member selection and executive management nomination/selection. As it pertains to a hospital CEO, hospital boards are responsible for evaluating and assessing executive performance as well as setting executive compensation.
The board has many fiduciary responsibilities but the two most important duties are ensuring patient safety/quality of care and evaluating the hospital chief executive officer. These board representatives contribute much to the hospital due to their backgrounds in finance, ethics, strategy, marketing, negotiations, fund raising and other important areas of expertise. Physician and nursing participation on hospital boards provides expertise on continuous quality improvement and higher quality of care [3-5]. As the single largest component of clinical staff, nurses directly interface with patients for the greatest percentage of time [6]. This gives them a unique awareness into the healthcare needs of the community [7]. Healthcare membership on hospital boards provides a patient care perspective on all board decisions such that patient safety and quality of care are not compromised.
Clinician Representation
Evidence supports the assertion that physician and other clinician board members greatly contribute to decision making in terms of quality of care, patient safety and overall health system performance [8]. Using Hospital Quality Alliance (HQA) and Hospital Compare data, a US Department of Health and Human Services database, on NFP hospitals in California, Gai and Krishnan documented that the absence of physicians on the board is associated with a decrease of 3 to 5 percentage points in 3 of 4 measures of care quality [9].
There are varying schools of thought regarding physician and nursing representation on hospital boards. The Joint Commission has explicitly stated that medical staff must collaborate with governing bodies (i.e. boards), chief executives and other senior management to achieve hospital goals [10]. However, they fell short of specifying the number or proportion of board members that should be medical staff. In a 2009 survey, the typical NFP hospital had between 14 and 17 board members, of which an average of 12 were independent (not hospital employees) and an average of 2 were physicians [11,12]. In a 2011 survey of 14 large hospital organizations, physicians comprised 14% of board members, nurses comprised 6% of board members and the remaining 80% were non-healthcare providers (Table 1) [13]. Among all 14 CEOs and 57 board members of these surveyed organizations, 59% of respondents stated that board deliberations would benefit from additional expertise. The total average number of physicians on hospital boards was 2.5 with a median of 1 in 2013 [14]. In 2015, these figures were 2.7 and 1 respectively, thus there has not been a significant change in physician representation on hospital boards over recent years. In a 2010 online survey of more than 1,000 physicians, 56% of respondents cited the lack of physician leadership/representation on the board as a reason for lack of trust in hospital relationships [15]. Furthermore, as previously cited, 59% of surveyed CEOs and board members state that board deliberations would benefit from additional expertise [13]. Increased healthcare provider representations on boards would increase both trust of hospital boards among healthcare providers and expertise in board deliberations. Medical staff representation on hospital boards shows a board’s willingness to engage and be responsive to the needs of physicians and nurses [16]. By having a seat at the board room table, this would facilitate clinician buy-in with regards to newly implemented policies and initiatives. At a time of sweeping healthcare reform, quality and safety are becoming more inextricably linked to hospital reimbursement. Physicians and nurses possess invaluable knowledge of clinical problems and practice, acquired through years of experience that informs hospital boards.
| Board composition in faith-based systems(n=179) | Board composition in secular systems(n=95) | Board composition inall systems(n=274) | |
|---|---|---|---|
| Nurses * | 16 (9%) | 2 (2%) | 17 (6%) |
| Physicians | 19 (11%) | 17 (18%) | 38 (14%) |
| Other80% | 143 (80%) | 76 (80%) | 219 (80%) |
| 179 (100%) | 95(100%) | 274 (100%) |
Table 1 Clinical composition of large system boards.
Reluctance to Increase Physician and Nurse Representation on Hospital Boards
A common cause of apprehension about the expansion of clinician membership on hospitals boards is the concern for conflicts of interest. The potential for conflict of interest is applicable to all boards members, clinician or not, and can be mitigated with careful selection of board members. Boards should take care to select clinicians who acknowledge that the fiduciary duty of boards is to fulfill its mission as opposed to satisfying a particularly stakeholder’s desires [16]. Boards should rigorously evaluate the relationships of clinicians with other organizations and possible competitors. This process can help eliminate clinicians with competing interests from being selected. Boards should select clinicians based on a broad scope of merit, such as prior leadership and management experience. This ensures that they have the requisite skill set to serve in a governance capacity. Such an example would be a physician who has served as a chief medical officer or medical staff president at a noncompeting hospital. Government regulations do restrict hospitals from packing boards with clinicians. An independent board free from influence is mandated by the IRS, federal and state laws. The recent Sarbanes-Oxley governance law requires the majority of board members and all members of compensation and audit committees to be independent, meaning they have to have no direct or indirect material conflict of interest. For this reason, many clinician board members are ex-officio (seated because of their position on the medical staff) non-voting members. However, this does not prevent them from speaking up in patient care and other issues important to physicians. Federal tax regulations require a NFP organization to declare on IRS Form 990 how many of the board's members are independent. This means that among other tests for being classified as independent, any such member must not receive direct compensation as an employee, or if they do, total compensation less than $10,000 as an independent contractor during that tax year. Most NFP hospital board members serve without compensation with only about 10-15% being compensated although government sponsored hospital compensate about 16% of board members [14,17]. The increasing employment of physicians by hospitals is creating a problem for hospitals that need independent directors on their boards. Since 80% hospitals are NFP, the IRS limits the membership of insiders (employed or active staff physicians) to less than half. The compensation committee, in particular, according to Section 4958 Rebuttable Presumption of Reasonableness criteria, cannot have physician insiders on it [18]. Hospital CEOs may also be concerned with increased access of physicians to board members, which may undermine the CEOs authority. One of the authors (BS) has been on a NFP hospital board and observed efforts to limit one-to-one access to board members for fear of mixed messaging or undue influence.
There is also some data suggesting that there is a negative relationship between donations to a hospital and physician representation [19].This is because the typical donor may not prefer the resource allocations in boards where physician and other clinician representation are high.
Selection of Physician Board Members
More than 90% of physicians surveyed by consulting firm PricewaterhouseCoopers said they should be involved in hospital governance, such as serving on boards to assist in performance improvement [15]. However, non-physician board members and administrative executives say most physicians lack the knowledge base, in-terms of leadership and business skills, to fully comprehend issues being debated at the board level. Simply being a good clinician does not put the physician at the same level as experienced board members. The other issue is that most, if not all, physicians must be taught a skill set very different from what is offered through a typical medical school curriculum. It is encouraging that an increasing number of physicians are earning their MBA, attending leadership programs or taking special courses in business so they can sit at the management or board room table and contribute to the partnership with other hospital board members, hospital executives and other senior managers [20]. There should be a more formalized process of training for physicians being recruited for board membership.
Another challenge in asking physicians to be part of a hospital board is the time commitment. While it is an honor to be asked to serve, if the physician decides to take the role seriously, the commitment to meetings, committees and special projects, such as CEO or new board members election, involves enormous time. This is particularly a problem if the physician does not have a vote, is expected to be a ‘rubber stamp’ or has an unpaid position.
Impact of Physician Employment by Hospitals
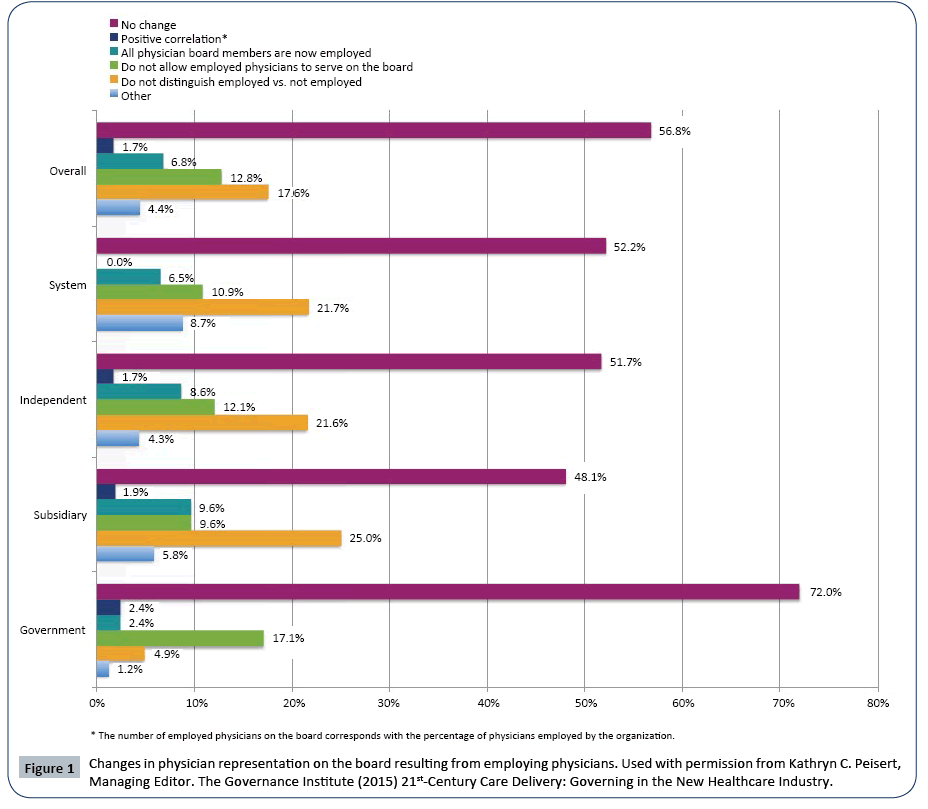
A recent survey of various types of hospital boards by the Governance Institute shows that over recent years there has been no change in physician representation in 57% of surveyed hospitals (Figure 1). 17.6% of hospitals do not distinguish between employed and non-employed physicians with respect to board membership and 13% do not allow employed physicians to serve on the board [14]. In a report about board composition in NFP hospitals, over half of survey respondents said there had been no change since the physician employment picture started to change [21]. 6.6% of responding NFP hospitals had a physician board chairperson while 72% had chairpersons with finance or business backgrounds.
In serial surveys by the Governance Institute, the proportion of voting directors who were medical staff physicians was 16.5% in 2007, 16.0% in 2009 and 17.3% in 2011 [22]. In a similar survey by Commonwealth Center for Governance Studies of 14 large health systems, 14% of board members were physicians, 6% nurses and the remainder was non-clinical persons [10].
Look at Hospital Boards in the Future
For many years, board appointments to hospitals have been ‘prestige’ appointments, meaning that prominent community members were asked to join, not necessarily based on their knowledge about healthcare or a specific set of skills important to the hospital, but because of their standing in the community. However, with the transformation in healthcare occurring every day, board members are being asked to have some knowledge and perspective about population health, compliance, regulatory changes, information technology, marketing, ethics, conflicts of interest, regulations, public relations and many other vital skills.
The future role of physicians on hospital boards is up for debate as to their presence and degree of representation. It may be that with increasing employment and alignment with hospitals that their primary role will be in executive positions, such as in a dyad role along with the CEO. In the value based care model, physicians add great expertise to the board in determining what adds value to healthcare delivery [23]. Physicians cannot generate work relative value units (a measure of value used in the US Medicare reimbursement formula for physician services) being on the board, participating in meetings and participating on committees, so there must be comparable compensation for their participation.
However, as pointed out, because of legal limitations, the hospital board may have to find retired physicians, physician leaders outside their own health system or physicians working in corporations and pay them for their service. In the current, as well as the future, environment, board composition will need very diverse governance skills, but clinical orientation of some members will be crucial to educating the rest of the board. It is clear that despite the changing healthcare environment, there has not been a significant change in physician representation on hospital boards even though the law allows, compensation and audit committees withstanding, for more physician and nursing representation. It is now time for more, not less, full voting physician members and other clinical experts on NFP hospital boards.
References
- Fast Facts on US Hospitals. Chicago (IL): American Hospital Association 2016.
- Prybil LD (2006) Size, composition, and culture of high-performing hospital boards. Am J Med Qual 21:224-229
- Weiner BJ, Alexander JA, Shortell SM (1996) Leadership for quality improvement in health care: empirical evidence on hospital boards, managers, and physicians. Med Care Res Rev 53: 397-416
- Jiang HJ, Lockee C, Bass K, Fraser I, Norwood EP (2009) Board oversight of quality: any differences in process of care and mortality? J Healthc Manag 54: 15-30
- Carman JM, Shortell SM, Foster RW, Hughes EF, Boerstler H, et al. (1996) Keys for successful implementation of total quality management in hospitals. Health Care Manage Rev 21: 48-60
- Barnet S (2014) 5 reasons hospital boards need more nurses. Chicago (IL): Becker’s Hospital Review 2014
- Nurses on Healthcare Boards. Chicago (IL): The American Hospital Association 2010
- Bader BS, Kazemek EA, Knecht PR, Witalis RW (2008). Physicians on the Board: Conflict over Conflicts. BoardRoom Press 2008
- Gai B, Krishnan R (2015) Do Hospitals Without Physicians on the Board Deliver Lower Quality of Care? Am J Med Qual 30: 58-65
- Bader BS, Kazemek EA, Knecht PR, Seymour D, Witalis RW (2010) Physician Participation on the Hospital Board: A Moving Target. BoardRoom Press.
- The Governance Institute (2009) Government structure and practices: Results, analysis and evaluation
- Prybil L, Levey S, Killian R, Fardo D, Chait R, et al. (2012) Governance in Large Nonprofit Health Systems: Current Profile and Emerging Patterns.Lexington (KY): Commonwealth Center for Governance Studies, Inc
- Gamble M (2012) What Does Governance Look Like in the Country’s Largest Health Systems? 8 Major Findings. Chicago (IL): Becker’s Hospital Review
- The Governance Institute (2015) 21st-Century Care Delivery: Governing in the New Healthcare Industry
- From courtship to marriage: A two part series on physician-hospital alignment PWC 2011
- Physicians on Hospital Boards: Time for New Approached. Chicago (IL): The American Hospital Association 2011
- Herman B (2016) Survey: 15% of Non-Profit Hospitals Compensate Board Members
- Code of Federal Regulations. Ithaca (NY): Cornell University 2016
- Brickley JA, Van Horn RL, Wedig GJ (2004) Board Composition and Nonprofit Conduct: Evidence From Hospitals. Rochester (NY): University of Rochester
- Satiani B, Sena J, Ruberg R, Ellison EC (2014) Talent management and physician leadership training is essential for preparing tomorrow’s physician leaders. J Vasc Surg 59: 542-546
- Gamble M (2013) Physician Representation on Health System Boards: 17 Findings. Chicago (IL): Becker’s Hospital Review 2013
- The Governance Institute (2012) Dynamic Governance: An Analysis of Board Structure and Practices in a Shifting Industry
- Totten MT (2011) Q&A: Physicians on Hospital Boards: Prepare to Challenge Traditional Wisdom. The American Hospital Association
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences