Rationalising Coagulation Test Orders in Emergemcy Department Wexford General Hospital
Muhammad Bilal, Yunitra Nedujchelyn, Hema N.Thuraisingam, Eoin Kelly, T. Paul Kelly, Muhammad Shahzad, Michael S. Molloy
DOI10.36648/2471-9781.21.7.285
Muhammad Bilal*, Yunitra Nedujchelyn, Hema N Thuraisingam, Eoin Kelly, T Paul Kelly, Muhammad Shahzad, Michael S Molloy
Department of Trauma and Critical Care, St Vincent University Healthcare Group, Elm Park, Dublin 4, Ireland
- *Corresponding Author:
- Muhammad Bilal
Department of Trauma and Critical Care, St Vincent University Healthcare Group, Elm Park, Dublin 4, Ireland
Tel: 00353851080460
E-mail: bilal_dr87@yahoo.com
Received Date: July 21, 2021; Accepted Date: August 12, 2021; Published Date: August 19, 2021
Citation: Bilal M, Nedujchelyn Y, Thuraisingam HN, Kelly E, Kell TP, et al. (2021) Rationalizing Coagulation Test Orders in Emergency Department Wexford General Hospital. J Hosp Med Manage Vol.7 No.8:285.
Introduction
Coagulation profiles are ordered for a variety of conditions in ED. Cost-effectiveness and efficiency are of increasing relevance in hospital medicine. Ordering unnecessary coagulation studies is of concern in a Model 3 hospital due to ineffective utilization of resources with limited laboratory staffing. Adherence to practical guidelines should help effect clinical decision making, resource utilization and cost savings [1].
Aim
To determine volume and appropriateness of coagulation tests ordered from ED
Methods
Chart review of attendances between 2nd-8th March 2020 where coagulation studies requested. Appropriateness was determined by reference to clinical guidelines developed by consultants in the department [2].
Results
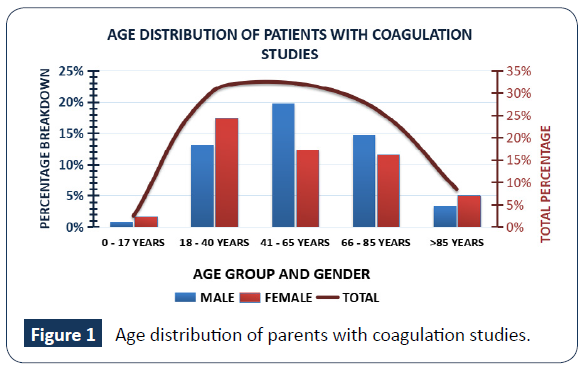
Age distribution of parents with coagulation studies (Figure 1).
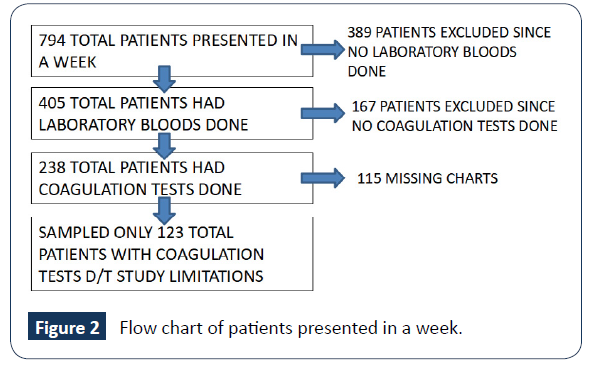
Flow chart of patients presented in a week (Figure 2).
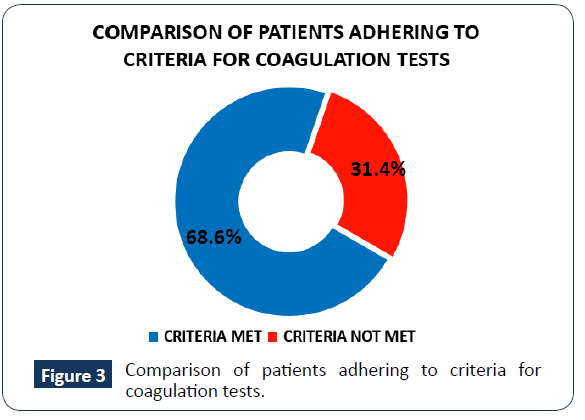
Comparison of patients adhering to criteria for coagulation tests (Figure 3).
Discussion
We found that there was no suitable indication for 68.6% of tests indicating significant wastage. The local cost for SINGLE coagulation test is 2.87 Euros [3]. Implementation of clinical guidelines, educational packages and/or algorithms in ED for nurses and physicians should reduce unnecessary coagulation testing [4]. This will enable effective utilization of laboratory resources as well as reduce financial cost. We desire at least 80% coagulation tests sent to be appropriate in Wexford ED thus further education and intervention is required [5].
Limitations
Limitations of the study includes missing charts; possibly being utilized for other audits or presentations; charts removed from ED for early pregnancy unit; misfiling or other reasons. This warrants further review and electronic scanning and warehousing of charts should be considered to avoid potential medico-legal consequences.
References
- Gupta R, Mondoux S, Rutledge G (2020) Reducing utilization of unnecessary coagulation tests by emergency providers. Can J Emerg Med 22: 55-56.
- Goldberg N, Chaudhry H, Ackery A, Sholzberg M (2017) Reduced Reducing Unnecessary Coagulation Testing in the Emergency Department. BMJ Qual Improv Rep 130: 55-81.
- Murphy E, Mac S, McGroarty C (2015) A novel approach to improving coagulation sample ordering in an emergency department. BMJ Qual Improv Rep 4: 22-25.
- Fralick M, Hicks LK, Chaudhry H (2017) Reducing Unnecessary Coagulation Testing in the Emergency Department. BMJ Open Quality 6: 161-165
- Boran G, Gaffney P, Condell S (2014) Sensible Test Ordering Practice in an Emergency Department Tallaght Hospital Dublin.
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences