Sudanese Male with Erosive Lichen Planus Case
Yousif I Eltohami, Nour E Alim and Amal H Abuaffan
DOI10.4172/2471-9781.100017
Yousif I Eltohami, Nour E Alim and Amal H Abuaffan*
Faculty of Dentistry, University of Khartoum, Sudan
- *Corresponding Author:
- Abuaffan AH
Faculty of Dentistry
University of Khartoum, Sudan
Tel: +249 91 778 8622
E-mail: amalabuaffan@yahoo.com
Received Date: November 25, 2016; Accepted Date: November 30, 2016; Published Date: December 02, 2016
Citation: Eltohami YI, Alim NE, Abuaffan AH. Sudanese Male with Erosive Lichen Planus Case. J Hosp Med Manage. 2016, 2:2.
Abstract
Lichen planus is a chronic mucocutaneous autoimmune disease, predominantly affects middle aged females, predisposing factors include psychological stress, drugs and various systemic conditions.
A case reports of Sudanese male 32 years old. Chief complain, burning sensation in the oral cavity associated with generalized pruritis, diagnosed as lichen Planus and had been treated with systemic prednisolone, topical analgesics and chlorhexidine oral rinse. The lesions showed excellent improvement within two weeks.
Keywords
Erosive lichen planus; Oral mucosa; Burning sensation; Systemic steroids; Prednisolone
Introduction
Lichen planus is a chronic inflammatory mucocutaneous disease, mainly affects the oral mucosa, when there is no associated cutaneous lichen planus or lichen planus at other mucosal sites it may called as “isolated” OLP. It is more common among middleaged group patient and more frequent in females [1]. Six clinical forms had been described by Andreason based on the clinical description of oral lesions; reticular, papular, plaque, atrophic, erosive and bullous. The most common one is reticular form with the characteristic feature of Wickham’s striate radiating from papules. Reticular, papular and plaque forms are asymptomatic but atrophic (erythematous), erosive (ulcerative) OLP is often associated with a burning sensation and pain [2]. Erosive lichen planus are symptomatic and carries an increased risk of developing into squamous cell carcinoma. Hence erosive OLP requires urgent treatment, a prompt palliation and meticulous follow up [3]. Here we report a case of erosive OLP affecting a middle-aged male.
Case Scenario
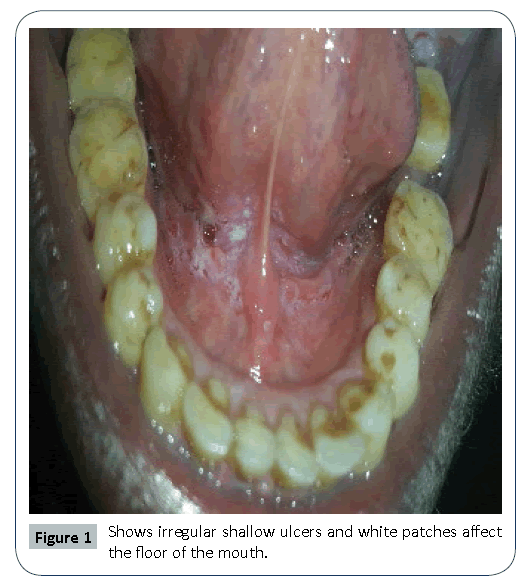
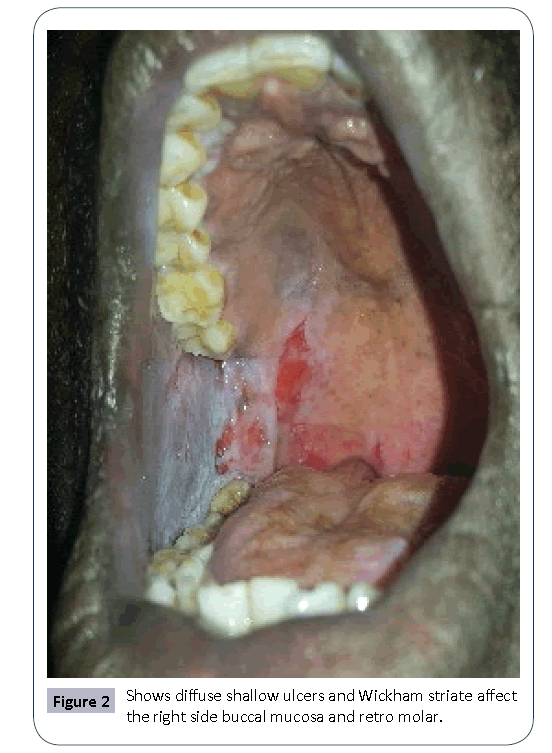
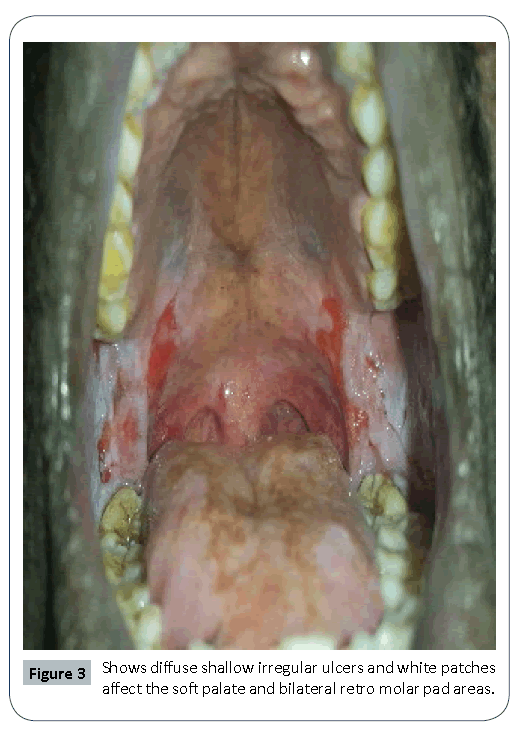
A 32 years old Sudanese male attended the Oral Medicine clinic complaining from severe burning sensation, difficulty in eating and swallowing in addition to taste changes started suddenly two months ago without previous episodes. No significant medical or social history. On Clinical examinations; tender, irregular, shallow, non indurate ulcers without apparent discharge and white patches & papules (Wickham striate) affected soft palate, floor of the mouth, bilateral buccal mucosa and retro molar pad areas and no obvious skin lesions (Figures 1-3). Histopathological examination revealed characteristic features of lichen planus without features of dysplastic changes. Patient was treated by chlorhexidine mouth wash, topical analgesics and high dose of oral systemic steroids (1 mg/kg). The treatment showed excellent improvement within two weeks, and then gradual tapering of the dose was recommended.
Discussion
Oral lichen planus (OLP) is a chronic mucocutaneous disease of unknown etiology The common age group affected ranges from the third to sixth life decades and mostly have female gender predilection, the cases of LP that are restricted to oral mucosa occur in 15% of all cases [4]. In contrast in the present case report the affected was Sudanese male which was not a common as in females and it was prominent only in the oral mucosa.
The etiology of OLP appears to be complicated and multi factorial. Ismail et al. [5] reported a list of causative and exacerbating factors for OLP and oral lichen planus reactions such as, drugs (anti-malarial, diuretics, gold salts, anti retroviral, beta blockers, pencil amine), dental materials (dental amalgam, composite and resin-based materials, metals), chronic liver disease and hepatitis C virus, genetics and tobacco chewing. In this case, there was no associated factor that may provoke oral lichen planus reaction. Stress was identified by previous studies as one of the most frequent causes of acute exacerbation of oral lichen planus [3,6], in the current case, patient denied any stressful conditions as predispose factor.In general the lesions in the oral cavity are multiple and bilateral [5-7]. It can be found in any area in the oral cavity, the buccal mucosa, gingiva and tongue were the main involved sites [5,6]. In the present case, the anatomical areas of the lesion were the floor of the mouth, soft palate, retro molar pads and buccal mucosa bilaterally. The lesions in the buccal mucosa had a striate shape and were reticulated, whitish, and those in the soft palate and retro molar area was erythematous. The malignant transformation potentiality for these lesions is still controversial. The frequency of malignant transformation ranges from 0.4% to 5%, with the highest rates in the erythematous and erosive lesions [3,5].
Diagnosis of OLP should hold by proper history, clinical examination and histopathological examination to confirm the clinical diagnosis and particularly to exclude dysplasia and malignancy [8]. The choice of treatment depends on the severity and the discomfort. Drugs are used to improve the condition of the patient it either local or systemic. The active components are corticosteroids such as triamcinolone, fluoc inolone acetonide and flocinonida. Ismail et al. reported that maintain of good oral hygiene enhance the healing and decrease the symptoms of OLP [5,9]. As in this case systemic steroids was resolute the lesions in two weeks accompanied by chlorhexidine mouth rinse.
Conclusion
OLP is an autoimmue disease which appears clinically in different types. The erosive lichen planus variant is one with highest malignant potentiality; hence it needs regular and meticulous follow up. It is important to identify the lesion clinically and Histopathological at the earliest and treat the condition in the early stage.
References
- Marzieh B, Narges G, Taghavi ZA, Mehdi V, Masoumeh M(2010) Review oral lichen planus. J Dent Res Dent Clin Dent Prospects 4:3-9.
- Andreasen JO(1968) Oral lichen planus 1. A clinical evaluation of 115 cases. Oral Surg Oral Med Oral Pathol 25:31-42.
- Einsen D(2002)The clinical features, malignant potential, and systemic associations of oral lichen planus: a study of 723 patients. J Am AcadDermatol46:207-214.
- Srinivas K, Aravinda K, Ratnakar P, Nigam N, Gupta S (2011) Oral lichen planus - Review on etiopathogenesis; Natl J Maxillofac Surg 2:15.
- Ismail SB, Satish KS and Zain RB (2007) Oral lichen planus and lichenoid reactions: etiopathogenesis, diagnosis, management and malignant transformation.J Oral Sci 49:89-106.
- Epstein JB, Wan LS, Gorsky M, Zhang L(2003) Oral lichen planus: progressin understanding its malignant potential and the implications for clinical management. Oral Surg Oral Med Oral Pathol Oral RadiolEndod 96:32-37.
- Scully C, Carrozzo M (2008) Oral mucosal disease: Lichen planus. Br J Oral Maxillofac Surg 46:15-21.
- Shetty P, Prashanth SK, Laxmikanth C, PrasannaK (2012) Erosive Lichen Planus-A Case Report. Pacific Journal of Medical Sciences9:53-56.
- Sousa FA, Rosa LE (2008) Oral lichen planus: Clinical and Histopathological considerations. Braz J Otorhinolaryngol 74:284-292.
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences