Terminal Cleaning Multi-Discipline Approach
Obedoza S, Bussiere KM and Simpkins R
DOI10.4172/2471-9781.100049
Obedoza S1, Bussiere KM2* and Simpkins R3
1BSN, CNOR, Director of Surgical Services, USA
2RN-CIC, Infection Preventionist/Occupational Health Nurse, USA
3Director of Environmental Services, USA
- *Corresponding Author:
- Bussiere KM
Infection Preventionist
Fort Washington Medical Center
Fort Washington, Maryland, USA
Tel: 7577175221
E-mail: kavvon@gmail.com
Received Date: March 09, 2018; Accepted Date: July 05, 2018; Published Date: July 09, 2018
Citation: Obedoza S, Bussiere KM, Simpkins R (2018) Terminal Cleaning Multi-Discipline Approach. J Hosp Med Manage Vol.4 No.1:5
DOI: 10.4172/2471-9781.100049
Preface
Fort Washington Medical Center has developed and implemented a multi-disciplinary approach to Terminal Cleaning of the Operating Room (OR) and all invasive procedural areas; we want to share the benefits and issues that were discovered by this process.
Background
What is a Terminal Clean? Many people not in healthcare assume that everything in the OR is sterile. This however, is not the case. Terminal Cleaning removes with a high degree of confidence all transmittable pathogens at the end of the day, so that the room starts at zero deficits for the first case of the next day. During the day there will be blood and tissue contamination of equipment and the environment as surgeries occur, along with site contamination from normal use and exposure to patients and staff. Between cases the Peri-operative team will remove any known or suspected contaminations and clean and disinfect high use objects, returning it to a near zero deficit for sequential cases. Terminal Cleaning is usually done after the case load ends allowing the cleaner to eliminate all the known and unknown threats. The Association of peri-Operative Registered Nurses (AORN) has national guidelines for removing all potential pathogenic harm from the ceilings, walls, floors, machines, tools, objects and furniture within the OR. We will not be discussing how to clean, as that is assumed as part of AORN standards. As far as who is doing the cleaning, it could be the Peri-op team, Environmental Services (ES), a contracted outside cleaning agency, or any combination thereof.
Clash of the Disciplines
Very often due to the disparity of roles between surgeons, anaesthesia, nursing, techs and ES- each coming with their own perspective and agenda- it is safe to say that friction is often generated between the disciplines. There are many ORs that run as smoothly as a Swiss watch in most respects, but may run into difficulties regarding who is responsible for validating a Terminal Cleaning. If ES is cleaning, the ES manager could validate but this could be seen as a lack of cross-auditing validation that regulatory agencies expect. ES could be assigned to the Peri-op team, but then no outside agent is observing Terminal Cleaning. Many facilities have put a Terminal Cleaning process in place without ever validating its efficacy.
Goals and Objectives
Our goals were to ensure that a Terminal Cleaning process occurred, was highly effective, was multi-disciplinary, and instilled a high degree of confidence. To start, Infection Prevention, Periop, and ES sat at the table to discuss a recent cleaning miss by EVS. While there we started to discuss how to prevent this in the future. Mostly we relied upon someone to report up the chain of command an infraction and then decide if the infraction was worth making it widespread to several departments. When we thought about that, it seemed like a failed process and that when we decided to create the process for Terminal Cleaning validation.
Methods and Materials
There are several ways to validate a Terminal Cleaning, the most expensive and time consuming is for ATP (Adenosine triphosphate) which can check for residual bio burden. Another option is to mark the specific objects with a bioluminescence marker, allow for the cleaning, then check to see if the luminescence was removed using a black light. This is repetitive and may lead to marked areas being targeted by ES workers. The third method is a visual inspection for cleanliness. This method is the least scientific, but the most easily recognizable by the Peri-op team as well as the quickest to perform. Ultraviolet disinfection does not validate terminal cleaning but is in itself a standard for effective disinfection and should be mentioned as an option.
Neither ES nor Peri-op wants to change their duties to include a Terminal Cleaning validation, but at the same time all want the process to change. Some questions for your facility to consider before implementing this process:
1. What does your facility have to work with for staff and products?
2. Can you afford the cost, the products and the time?
3. Can you afford not to validate your processes?
4. What is being missed by not validating Terminal Cleaning?
5. What can you put into practice that can be maintained and sustained?
Deciding on a Process
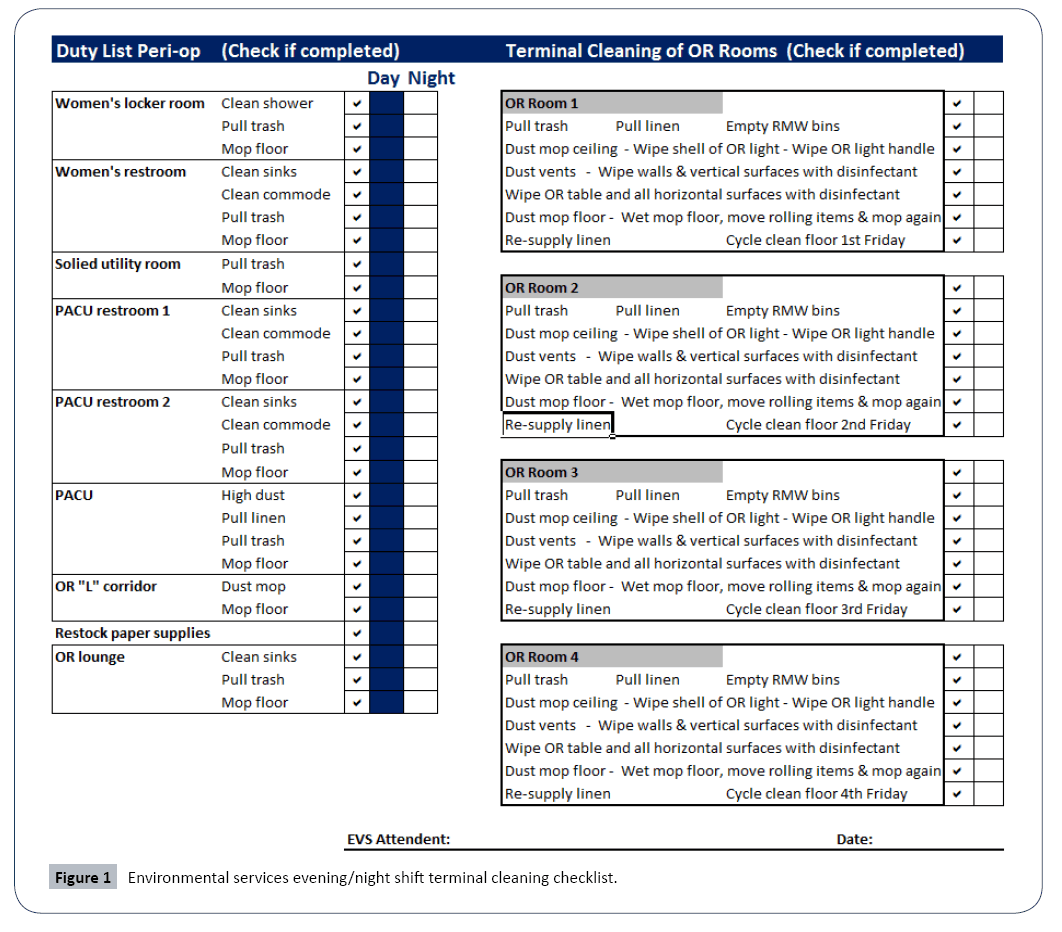
The multidisciplinary team created a very specific checklist for ES to use to perform the Terminal Cleaning: one for the day shift while active cases are taking place and a second for the evening/night shift when Terminal Cleaning and other duties occurred. A checklist for the Peri-op team was also created to use prior to setting up for the first case, where they would visually inspect the room for cleanliness. These checklists were forwarded to the Infection Preventionist to enter the information into a spread sheet or database. Creating this process helped identify and address failures, but also allowed the system to keep moving forward and eliminated blame. This allowed the multidisciplinary team to repair Terminal Cleaning failures prior to the first case starting; sometimes a slight delay would occur, but not without inspiring confidence that the room would be starting at zero deficits. The surgeons were on board with this but it threw the Anaesthesiologist schedule off and they had to re-adjust.
Training occurred for all three disciplines. To ensure that we started with a knowledge base sufficient for the task, we brought in an outside firm from an ES product company that also specializes in Peri-op cleaning to instruct ES workers on the Terminal Cleaning process. The Peri-op had to become consistent with their expectations with cleaning. They were marking everything compliant even if it had to be re-cleaned due to favouritism with ES workers. Infection Prevention added management of the checklist data to their workflow. This was taking the daily checklists and compiling them into a monthly and yearly report (Figure 1).
The Initial Results
It’s wonderful to be perfect. The ES checklists and the Peri-op validations were both 100% completed during the first testing cycle. Being sceptical, the Infection Preventionist went to the OR, dressed in scrubs, and inspected the OR rooms against the checklist. There were still missed areas and items that were marked on the checklist as completed.
In discussing with both parties, each was afraid to enter anything but 100% assuming there would be negative consequences. The multidisciplinary team sat down with the frontline staff and discussed transparency, to stress the need to report correctly as a first step to improvement. Staff then complied with being transparent with the checklists and some issues were identified. The team was able to determine the root cause of the deficits and this resulted in changes in practice, notifications, product, and training. Staff was not disciplined for being transparent. This increased the trust across the disciplines and allowed for a tighter control in communications.
Using the PDCA Cycle
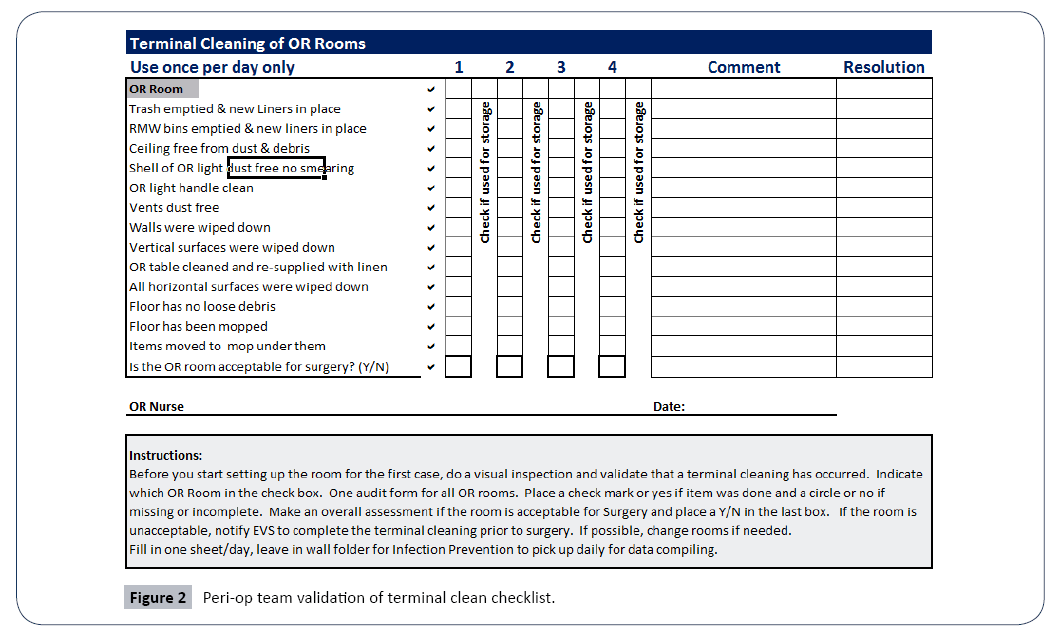
The team used the PDCA cycle to improve the checklists by asking the ES workers & Peri-op team for feedback on the process. The answer was a simple change in the form so that one member of the Peri-op team could check all their rooms on one checklist and mark when the OR was used for storage only (Figure 2).
Process Improvement
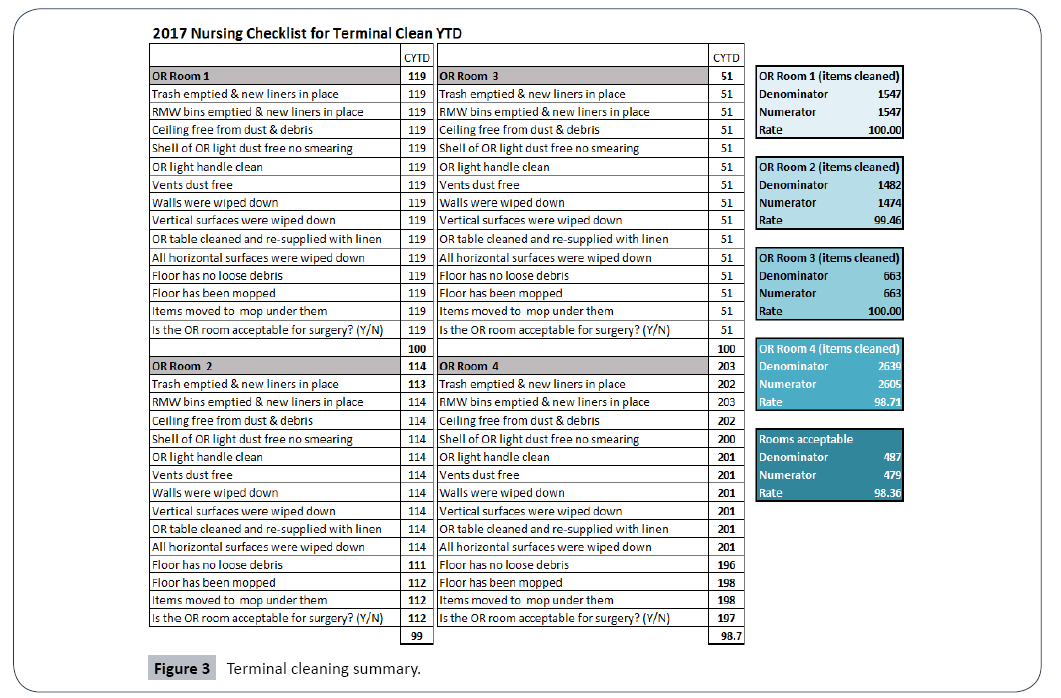
The compiled monthly results from the checklists are presented at the Surgical Executive Committee and a yearly summary is presented at the Infection Prevention & Control Committee. Information from both of these committees is forwarded up to the Medical Executive, QAPI, and Performance Improvement Committees to share with all key stakeholders. For QAPI, there are measurable goals for both Peri-op and Environmental Services to report.
Surgical Executive committee would correlate the delay in starting cases with any of the Terminal Cleaning failures. Infection Prevention would be reporting both the consistency of the cleaning process, correlation to any SSI cases and overall cleanliness issues that persist (Figure 3).
Validation Training and Competency
After holding the initial training for ES, sequential new hires are trained by preceptor ship of a previously trained ES worker using the checklists. We can call for repeat training from an outside source on Terminal Cleaning if needed. We hold the Peri-op staff accountable for completing the checklists and dealing with outliers such as vacations, staffing, late surgical cases, etc. If there are missed days or delays Infection Prevention escalates it to the Peri-op Director.
Constructively using the Results
For the Peri-op team, there is an increased confidence in the Terminal Cleaning process and they have ownership within the validation process.
For Environmental Services, there is the ability to hone in on who needs more training. Product changes can be tested in this process with measurable goals.
For Infection Prevention, any SSI investigation can reflect on the checklist to determine if a Terminal Cleaning was done prior to the surgery.
Conclusion
This process has led to a greater cohesiveness with which ES & Peri-op work together to build higher confidence in Terminal Cleaning. The validation that Terminal Cleaning occurred and occurred properly is working well with the current process. Staff feels secure to be honest and transparent which has led to improvements in the Terminal Cleaning process. Consistent documentation gives strength and support when crossing disciplines with corrective issues. A noted limitation is the need for outside validation to ensure both parties are accurately cleaning and documenting through a spot check process via bioluminescence or ATP.
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences