Ultrasound Guided Femoral Nerve Blocks and the Management of Elder Patients with Hip Fractures
Jessica Bates,Suzanne Michelle Rhodes, Richard Amini
DOI10.4172/2471-9781.100004
Jessica Bates, Suzanne Michelle Rhodes and Richard Amini*
Department of Emergency Medicine, The University of Arizona College of Medicine, Tucson, AZ, USA
- *Corresponding Author:
- Richard Amini
MD, Department of Emergency Medicine
The University of Arizona College of Medicine
Tucson, AZ, USA
Tel: +1 520-626-4555
E-mail: RAmini@aemrc.arizona.edu
Received Date: October 26, 2015; Accepted Date: December 08, 2015; Published Date: December 15, 2015
Abstract
Hip fractures in the elder population are not infrequent and often result in untreated pain or large quantities of opioid administration. Femoral nerve blocks (FNBs) offer a safe, effective method for improving pain control in the setting of hip fracture, which can be initiated in the emergency department (ED). The use of ultrasound has been shown to improve efficiency and accuracy of FNB with an added benefit of reducing the volume of local anesthetics utilized compared to landmark technique. Prior studies have shown that ultrasound training for FNB proficiency can be easily accomplished in the ED setting. There are relatively few known complications associated with FNBs and published studies on ultrasound-guided FNBs have reported zero complications. After reviewing the available literature, we believe the emergency physician is well suited to perform ultrasound guided FNBs; which will lead to improved pain control, decrease opioid requirements, and can potentially reduce medication-induced delirium in the elder population requiring lower extremity pain control.
Keywords
Femoral nerve blocks; ED setting; Hip fractures; Opioid; Medicationinduced delirium
Introduction
Hip fractures are a common injury in the elder population with over 250,000 cases in 2010 occurring in patients of age 65 and older [1]. Hip fractures are estimated to cost nearly 2.9 billion dollars per year [2]. Adding to these costs are the potential problems that can complicate elder patients’ hospital course such as urinary tract infections and the development of delirium. In fact, delirium in elder patients who are admitted to intensive care units has been demonstrated to increase mortality by 26% when compared with those elder patients who do not develop delirium [3]. Several hypotheses exist as to why elder patients develop delirium such as poly-pharmacy, poor control of pain, environmental changes or direct opioid side effects; however there has been no overwhelming evidence to support one hypothesis over another [4,5]. Several studies have been conducted demonstrating the feasibility of femoral nerve blocks (FNBs) from the emergency department [5-10]. Furthermore, numerous studies demonstrate improved pain control and decreased opioid use with implementation of femoral nerve blocks [11,12]. Despite the evidence, institutions often face difficulties when implementing FNB protocols. In fact, Holdgate et al. revealed that of 36 emergency departments in Australia, in patients who presented with hip fracture (n = 645), only 7% received a FNB [13]. Moreover, Mittal and Vermani conducted a national survey in the United Kingdom (UK) and found that 74% (n = 230) of the UK EDs contacted had ultrasound access. However, only 10% regularly administered ultrasound guided FNBs [14]. In this review, we summarize the use and benefits of FNBs, particularly with regard to hip fractures in the elder population. We also aim to highlight a need for further research into the possible reduction of delirium in the elder population.
Methods
This manuscript is a miniature review and has been conducted at an academic medical center. We searched the current literature available on Cocharane Database and PubMed using combinations of the terms, “ultrasound guided”, “femoral nerve block”, “threein- one nerve block”, “hip fracture”, “femoral fracture”, “elderly”, “elder”, “delirium”, and “pain control.” Authors are emergency medicine physicians with experience in emergency ultrasound. Author JB is a third year resident with training in education, author SMR is fellowship trained in hospice and palliative medicine, and author RA is fellowship trained in emergency ultrasound and is a registered diagnostic medical sonographer.
Utility of femoral nerve blocks
FNBs have been used in clinical practice for decades by emergency physicians, orthopedists and anesthesiologists. The clinical applications of FNBs include lacerations to lower extremities, patellar injuries, femoral fractures and hip fractures [6,15-18]. In 2003, emergency department driven research by Fletcher et al demonstrated that FNBs confer improved pain relief when compared to opioid therapy alone [6]. In 2008, orthopedic research performed by Mutty et al demonstrated improved pain management when patients with hip fractures underwent femoral nerve blocks in the emergency department [7]. The Cochrane database last visited this topic in 2003 and their consensus summary states that femoral nerve blocks have been shown to decrease pain in patients with hip fractures when the FNB is performed both in the acute and preoperative setting [19]. Finally, in 2013, a randomized control trial was conducted and demonstrated that patients who received FNBs consistently required less pain medications [16]. There are clear benefits to using FNBs to improving pain and decreasing opioid requirement in patients with femoral and hip factures.
Ultrasound improves nerve blocks
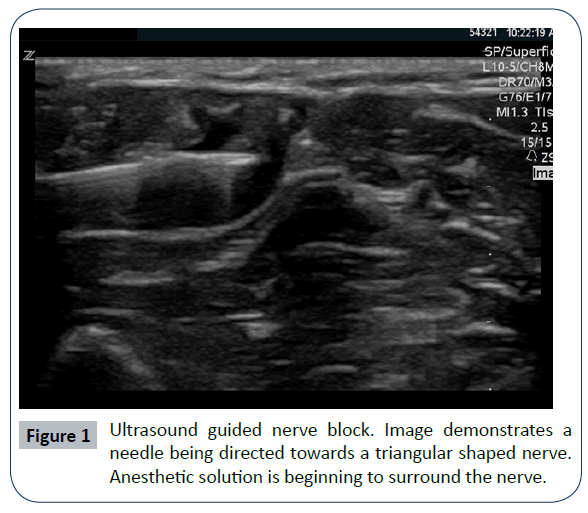
Femoral nerve blocks can be performed using any of the following techniques: anatomical landmarks, nerve stimulators, and ultrasound guidance (Table 1). However, in 1997, Marhofer et al confirmed that ultrasound guided FNBs were statistically superior to nerve stimulator technique in both time of onset and efficacy of procedure [11]. Despite the positive consensus in the literature and across numerous medical specialties, femoral nerve blocks are not being used on a regular basis for pain control in patients with hip fractures [14,15]. Two commonly encountered barriers to implementing FNB protocols include the arguments that FNBs are technically challenging; and that FNBs are associated with complications. The use of point of care ultrasound is a skill that alleviates both challenges and is currently being taught in nearly all specialties. Ultrasound provides a mechanism by which clinicians can directly visualize fascia, vasculature, and nerve. This allows a clinician the ability to guide the needle and safely insert anesthetic solution around the nerve (Figure 1). Various studies have been conducted to demonstrate the ease and safety of performing ultrasound guided FNB [15,16,20-22]. Anesthesia and Emergency Medicine literature has demonstrated ultrasound guided FNBs can lead to faster and improved quality of nerve blocks [9,11,16,20,21]. Lastly, when ultrasound is used, less anesthetic is used to achieve adequate blockade [16,19,23].
Table 1: Comparison of techniques used for Femoral Nerve Blocks [6,7,10-12,16,21,23,24].
| Advantages | Disadvantages | |
|---|---|---|
| Blind FNB | Can perform in situations without access to ultrasound | Anatomical variation/obese patients increase complications Increased use of local anesthetic compared to NS and US FNBs |
| Nerve Stimulator (NS) FNB | Improved quality compared to blind FNB | Longer time to onset Increased local anesthetic requirement compared to US FNB |
| Ultrasound (US) Guided FNB | Shortest time to onset Least amount of local anesthetic required Greatest quality of pain relief Fewest complications |
Requires access to US |
Ultrasound guided femoral nerve block training
A common teaching model in medicine comes from the paradigm “see one, do one, teach one.” In medicine, one of the biggest barriers to teaching technically challenging procedures is the lack of direct feedback. When a senior resident or attending cannot see what the junior is doing, anxiety can lead to complications or worse, decreased teaching. When conducting ultrasound guided techniques, senior physicians can be confident in the progress of the procedure because both parties can “watch” the needle as it is directed. Due to ultrasound guidance, performing femoral nerve blocks are now no more difficult or technically challenging that performing an ultrasound guided internal jugular central line where the needle is within millimeters from the carotid artery.
Review of the literature demonstrates that ultrasound guided FNBs can feasibly be taught in the emergency department setting [8,9]. In 2012, a study conducted from the emergency department by Haines et al. demonstrated the ease of learning ultrasound guided femoral nerve blocks by emergency physicians [10]. In fact, emergency medicine residents and attending physicians proved proficient after a 30min lecture and practice on mannequin or real patient. In this study, the supervising ED physician declared a physician competent when the physician was able to successfully conduct femoral nerve blocks on a real patient without requiring assistance [10]. Furthermore, Akhtar et al. demonstrated in 2013 that a one hour training module consisting of didactic lecture and hands-on demonstration on FNBs yielded high competency rates in first year emergency medicine residents both immediately and at three months. A post-test as well as “critical actions checklist” under direct observation of a FNB were utilized to assess competency. After the initial teaching module, 37 of 38 (97%) residents were deemed competent in performing a FNB and at three months, 83% maintained proficiency [8].
Femoral nerve block associated complications
Unlike complex and high-risk procedures, such as central line placement or anatomical landmark guided subclavian central line placement where the clinician is millimeters from an artery and risks complications such as arterial puncture, pneumothorax, and dysrhythmia; femoral nerve blocks under ultrasound guidance are always performed in long axis approach whereby the user directly visualizes the entire length of the needle as it approaches the nerve. Complications that have been associated with femoral nerve blocks include lidocaine associated local anesthetic systemic toxicity (LAST), direct nerve damage, and infections. Although the potential for these complications exists, they are rare. In fact, a study conducted in 2003 used the anatomical landmark technique and encountered zero complications out of 50 FNBs performed [6]. In 2010 and 2013, ultrasound guidance was used and out of 28 combined nerve blocks performed all were successful and zero had complications [15,16].
Emergency department role
Emergency physicians are the ideal clinicians to care for the pain management of elder patients, because they are the first physicians to assume the care for these patients and can more quickly address pain control. Fletcher et al. found that patients who were administered a FNB reached their lowest pain score in 2.88 hours versus 5.81 hours in the control group receiving intravenous morphine [6]. Currently, emergency physicians are trained extensively on the use of bedside ultrasound and emergency programs across the country are further developing their ultrasound divisions for the purpose of increasing training and improving patient care. There is still room for improvement, however, as a survey of 242 EDs in five states (Arkansas, Hawaii, Minnesota, Vermont, and Wyoming) found that only 47% of non-academic EDs had point-of-care ultrasound immediately available [24]. The growing number of ultrasound programs has quality assessment means as well as a structured approach to credentialing and documentation [25]. Emergency physicians use the ultrasound to insert central lines, to perform needle guided aspirations of tonsils and peritoneal cavities, and to guide needles into joint spaces in addition to an increasing number of nerve blocks, including FNBs. Certainly a multispecialty approach is necessary and collegial communication is required for the care of elder patients [26]. However, as the evidence of FNBs builds; failing to perform femoral nerve blocks when indicated may soon be negligent.
Conclusion
We have discussed the benefits of clinical application of ultrasound guided FNBs in the setting of hip fracture in the elder population. Multispecialty efforts must be endeavored to improve patient care and decrease the potential for medication-induced delirium in the elder population. Femoral nerve blocks, which can be initiated in the emergency department, can improve pain control in patients with hip fractures and can lead to decreased use of opioid medications.
References
- Bekkers S, Bot AG, Makarawung D, Neuhaus V, Ring D (2014) The National Hospital Discharge Survey and Nationwide Inpatient Sample: the databases used affect results in THA research. ClinOrthopRelat Res 472: 3441-3449.
- (CDC) CfDCaP (1996) Incidence and costs to Medicare of fractures among Medicare beneficiaries aged greater than or equal to 65 years--United States, July 1991-June 1992. MMWR Morb Mortal Wkly Rep 45: 877-883.
- LahariyaS, Grover S, Bagga S, Sharma A (2014) Delirium in patients admitted to a cardiac intensive care unit with cardiac emergencies in a developing country: incidence, prevalence, risk factor and outcome. Gen Hosp Psychiatry 36:156-164.
- Vaurio LE, Sands LP, Wang Y, Mullen EA, Leung JM (2006) Postoperative delirium: the importance of pain and pain management. AnesthAnalg 102:1267-1273.
- Morrison RS, Magaziner J, Gilbert M,Koval KJ, McLaughlin MA, et al. (2003) Relationship between pain and opioid analgesics on the development of delirium following hip fracture. J Gerontol A BiolSci Med Sci 58:76-81.
- Fletcher AK, Rigby AS, Heyes FL (2003) Three-in-one femoral nerve block as analgesia for fractured neck of femur in the emergency department: a randomized, controlled trial. Ann Emerg Med 41:227-233.
- Mutty CE, Jensen EJ, Manka MA Jr, Anders MJ, Bone LB (2007) Femoral nerve block for diaphyseal and distal femoral fractures in the emergency department. J Bone Joint Surg Am 89:2599-2603.
- Akhtar S, Hwang U, Dickman E, Nelson BP, Morrison RS, et al. (2013)A brief educational intervention is effective in teaching the femoral nerve block procedure to first-year emergency medicine residents. J Emerg Med 45:726-730.
- Christos SC, Chiampas G, Offman R, Rifenburg R (2010) Ultrasound-guided three-in-one nerve block for femur fractures. West J Emerg Med 11:310-313.
- Haines L, Dickman E, Ayvazyan S, Pearl M, Wu S, et al. (2012) Ultrasound-guided fascia iliaca compartment block for hip fractures in the emergency department. J Emerg Med 43:692-697.
- Marhofer P, Schrogendorfer K, Koinig H, Kapral S, Weinstabl C, et al. (1997)Ultrasonographic guidance improves sensory block and onset time of three-in-one blocks. AnesthAnalg 85:854-857.
- Abrahams MS, Aziz MF, Fu RF, Horn JL (2009) Ultrasound guidance compared with electrical neurostimulation for peripheral nerve block: a systematic review and meta-analysis of randomized controlled trials. Br J Anaesth 102:408-417.
- Holdgate A, Shepherd SA, Huckson S (2010) Patterns of analgesia for fractured neck of femur in Australian emergency departments. Emerg Med Australas 22:3-8.
- Mittal R, Vermani E (2014) femoral nerve blocks in fractures of femur: variation in the current UK practice and a review of the literature. Emerg Med J 31:143-147.
- Beaudoin FL, Nagdev A, Merchant RC, Becker BM (2010) Ultrasound-guided femoral nerve blocks in elderly patients with hip fractures. Am J Emerg Med 28:76-81.
- Beaudoin FL, Haran JP, Liebmann O (2013) comparison of ultrasound-guided three-in-one femoral nerve block versus parenteral opioids alone for analgesia in emergency department patients with hip fractures: a randomized controlled trial. AcadEmerg Med 20:584-591.
- Kim YM, Kang C, Joo YB, Yeon KU, Kang DH, et al. (2015) Usefulness of Ultrasound-Guided Lower Extremity Nerve Blockade in Surgery for Patellar Fracture. Knee SurgRelat Res 27:108-116.
- Choi JJ, Lin E, Gadsden J (2013) Regional anesthesia for trauma outside the operating theatre. CurrOpinAnaesthesiol 26:495-500.
- Parker MJ, Griffiths R, Appadu BN (2002) Nerve blocks (subcostal, lateral cutaneous, femoral, triple, psoas) for hip fractures. Cochrane Database Syst Rev Cd001159.
- Bhoi S, Sinha TP, Rodha M, Bhasin A, Ramchandani R, et al. (2012) Feasibility and safety of ultrasound-guided nerve block for management of limb injuries by emergency care physicians. J Emerg Trauma Shock 5:28-32.
- Reid N, Stella J, Ryan M, Ragg M (2009) Use of ultrasound to facilitate accurate femoral nerve block in the emergency department. Emerg Med Australas 21:124-130.
- Williams R, Saha B (2006) Best evidence topic report. Ultrasound placement of needle in three-in-one nerve block. Emerg Med J 23:401-403.
- Casati A, Baciarello M, Di Cianni S, Danelli G, De Marco G, et al. (2007) Effects of ultrasound guidance on the minimum effective anaesthetic volume required to block the femoral nerve. Br J Anaesth 98:823-827.
- Sanders JL, Noble VE, Raja AS, Sullivan AF, Camargo CA (2015) Access to and Use of Point-of-Care Ultrasound in the Emergency Department. West J Emerg Med 16:747-752.
- Stein JC, Nobay F (2009) Emergency Department Ultrasound Credentialing: a sample policy and procedure. J Emerg Med 37:153-159.
- Johnson B, Herring A, Shah S, Krosin M, Mantuani D, et al. (2014) Door-to-block time: prioritizing acute pain management for femoral fractures in the ED. Am J Emerg Med 32:801-803.
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences