Virtual Teams in Academic Medicine in the COVID-19 Pandemic Era
Anish Bhardwaj
Department of Neurology, University of Texas Medical Branch (UTMB), Galveston, Texas, USA
Received Date: 2022-04-01 | Published Date: 2022-04-29DOI10.36648ͬ2471-9781.8.4.311
Anish Bhardwaj*
Department of Neurology, Neurosurgery, Neuroscience, Cell Biology and Anatomy, University of Texas Medical Branch (UTMB), Galveston, Texas, USA
- *Corresponding Author:
- Anish Bhardwaj
Department of Neurology, Neurosurgery, Neuroscience, Cell Biology and Anatomy, University of Texas Medical Branch (UTMB), Galveston, Texas, USA
E-mail:anbhardw@UTMB.EDU
Received date: April 1, 2022, Manuscript No. IPJHMM-22-12925; Editor Assigned date: April 4, 2022, PreQC No. IPJHMM-22-12925(PQ); Reviewed date: April 19, 2022, QC No. IPJHMM-22-12925; Revised date: April 25, 2022, Manuscript No. IPJHMM-22-12925(R); Published date: April 29, 2022, DOI: 10.36648ͬ2471-9781.8.4.311
Citation: Anish Bhardwaj (2022). Virtual Teams in Academic Medicine in the COVID-19 Pandemic Era. J Prev Med Vol.8 No.4:311
Abstract
Historically, teamwork has been the cornerstone of academic medicine’s “tripartite” mission of clinical service, teaching and training, and research and scholarship. With tectonic changes in healthcare with concomitant socio-cultural-economic, environmental, and generational influences; demographic shifts; dearth of workforce; burgeoning data; and technological advances; several tools (group support systems, team websites, e-mail, instant messaging, and videoconferencing) have advanced the concept and practice of teamwork via virtual team constructs. The challenges associated with the COVID-19 pandemic have escalated the utility of virtual teams in Academic Medical Institutions (AMIs), which are likely to play a dominant role in their repertoire in the foreseeable future. This treatise critically examines the evolution of virtual teams, expounds on their advantages and disadvantages, and posits a paradigm shift in teamwork toward provision of continued excellence in clinical care, discovery, innovation and developing the next generation of clinicians, educators, scholars and researchers.
Introduction
"Teamwork is the ability to work together toward a common vision. The ability to direct individual accomplishments toward organizational objectives. It is the fuel that allows common people to attain uncommon results." -Andrew Carnegie
From the humble beginnings of academic medicine in the U.S. in 1781 at the University of Pennsylvania, Academic Medical Institutions (AMIs) have evolved into highly complex multifaceted Healthcare Organizations (HCOs) with ever-increasing footprints resulting from mergers and acquisitions. Many of these AMIs operate via manifold matrix governance constructs that have enormous heterogeneity with cumulative diversity of workforce that have intricate internal as well as environmental modulatory influences [1-4]. Congruence between various entities is critical toward fulfilling the academic mission of AMIs to provide excellence in clinical care, teaching and training, and research and scholarship, along with community engagement, diversity, and inclusion [5-8]. Teamwork is paramount in providing comprehensive multidisciplinary clinical patient care and has growing importance in collaborative basic science and clinical research (“team science”), interactive education, training, and mentoring (“team mentoring”) [9,10]. Over the past few decades, with rapid advancements in communication technologies, there has been a gradual but evolutionary shift toward application of virtual teams in our armamentarium as it applies to the mission(s) of AMIs. This treatise provides a historical perspective emphasizing the importance of team constructs and teamwork (physical and virtual) in overcoming the formidable challenges in realizing the intended mission(s) of AMIs. It highlights the advantages and challenges encountered with virtual teamwork that is being increasingly utilized especially in the era of the COVID-19 pandemic.
Historical perspective on teams and teamwork in AMIs
The utilization of teams in AMIs has evolved greatly over the past century. “Task performance” has its origins in the industrial revolution (1760-1840) where enhancing operational efficiencies in production systems helped streamline manufacturing jobs into smaller, simpler, more manageable interconnected activity subunits with managers and professionals working cooperatively [11,12]. Team constructs were obligatory for more complex tasks that entailed brisk change, with concomitant shift from productivity to quality and customer service. The famed “Hawthorne studies” focused attention on the social and environmental influences on team performance [13]. In the 1960s and 1970s, organizational psychologists and industrial engineers proposed using teams for technically inexact, complex and inter-reliant jobs necessitating synchronization as well as tractability in an uncertain milieu. The current emphasis on teamwork was augmented by the rise of industries in Japan and was subsequently adopted by establishments in the U.S. and Europe, with a focus on quality improvement and with matching teams of production workers and supervisors who focused on evaluating problems and recommending concrete solutions. It was noted that teamwork enhanced operational outcomes through synergies that augmented individual performance. Zigurs’s research further supported the role and opportunities for virtual teams [14]. With increasing environmental complexity and globalization, conventional organizational hierarchies have iteratively resorted to teamwork with a focus on dynamic team composition, communication technology, empowerment, delayering, and diversity [15].
Deeply rooted in the clinical care of the wounded on the battlefield, these concepts of teamwork have long been extrapolated to healthcare provision in the realm of operative procedures, and in the advent of specialization among physicians (e.g., infectious diseases, endocrinology, neurology, general surgery, etc.), in nursing, and in other allied health professions (e.g., pharmacists, nutritionists, physical therapists, etc.). A plethora of studies in the literature show that cohesive well-coordinated teamwork enhances patient outcomes towards the overarching goals articulated by the institute of medicine (i.e., safe, effective, patient-centered, timely, efficient, and equitable patient care) [16,17] of note, the healthcare industry is the largest employer in the U.S., with healthcare costs ~ 19% of gross national product [18]. Commensurately, with over 150 medical schools in the U.S., AMIs have incrementally and increasingly become complex matrix organizations over the past few decades. Typically, such institutions have a medical school, one or more hospitals, ambulatory clinics, rehabilitation services, basic science, and clinical research facilities. Employees include trainees (undergraduate medical and graduate students, residents, and post-doctoral fellows), faculty (clinical, research, and teaching), healthcare providers, and administrators. Consequently, team building and teamwork among clinicians, researchers, and educators have become more than ever vital in advancing the “tripartite” mission of academic medicine.
Communication technologies
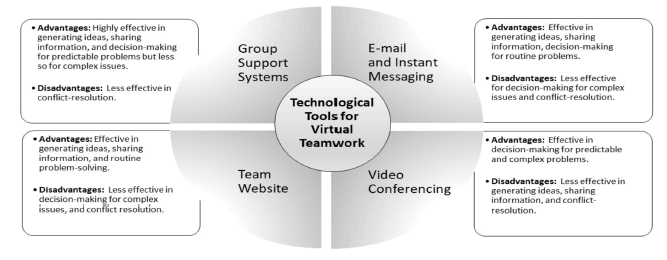
While decision-making involving face-to-face meetings have been the prevailing norm for decades, with advancements in communication technologies, meetings have evolved into virtual teamwork [2]. Selecting the right communication technology has depended on the characteristics of the technology, the task at hand, and the construct of two-member (physician-administrator “dyads”) or multi-member teams [5]. This is because utilizing the most advanced technology may not necessarily be paramount, given that more robust technologies can be distracting and perplexing. Over time, teams have learned to adapt to these tools through their modification and by developing new communication norms and procedures that are task specific. Group Support Systems (GSS) are information systems that emerged in the 1980s, subsequently migrating to the Internet, and include project management systems that are typically used for team-based support (e.g., scheduling and monitoring) [19]. Other GSS include file sharing, workflow support, teleconferencing, and group decision support systems. Additional technological tools such as team website, e-mail, and instant messaging, are useful for generating ideas, sharing information, and decision-making for predictable problems, but are less so for complex issues. By comparison, videoconferencing is relatively less effective in engendering ideas and information-sharing. One of the foremost limitations of these virtual systems is their ineffectiveness in conflict resolution due to the modulation of interpersonal effects with a propensity to augment negative or emotionally charged messaging (by reducing status differences, diffusion of interactions with some degree of anonymity among participants, and by attenuating social and emotional cues) (Figure 1) [12,20]. Many of these consequences reveal the dearth of communication norms for regulating acceptable behavioral conduct in these contexts.
In the clinical realms, telehealth and telemedicine have garnered renewed interest, in rendering patient care through virtual visits that afford “high quality care at a low cost” by enhancing access to care for those in rural areas, those with transportation barriers, and those encountering provider shortages in several subspecialties (e.g., mental health, rehabilitation medicine, dermatology, consultative services, nutrition management, etc.) [21,22]. The challenges for virtual patient visits center around evidence-based outcomes including quality, specific target patient demographics that benefit from this modality, and legislative policies for reimbursement for such services from third-party payers.
In the domain of education and training, virtual classrooms, lectures, and conferences, are being offered through webinars increasingly using pre-recordings and live videoconferencing. More and more, faculty and other healthcare professionals in AMIs are engaged in interprofessional collaboration in the domains of research, scholarship, mentoring, and career development across departments in and across other AMIs by overcoming the barriers of location, time and distance [23-25]. Key considerations in formulating virtual teams via collaborative models include stages of forming (group goal setting), storming (group negotiations for expectations), norming (building group trust and accountability), and performing (group productivity) toward ensuring lasting success.
Team performance with virtual teams
With ever-expanding inter-institutional and transnational research collaborations, and newer communication and collaborative technologies that enhance access to data and information, time and geographical location no longer impede virtual team meetings. Rapidly developing communicating technologies (e.g., video, skype, etc.) as a function of their interactivity, value, alacrity, and capability to record communications, have enhanced access to information as well as supported internal and external communication to augment team tasks and processes [12].
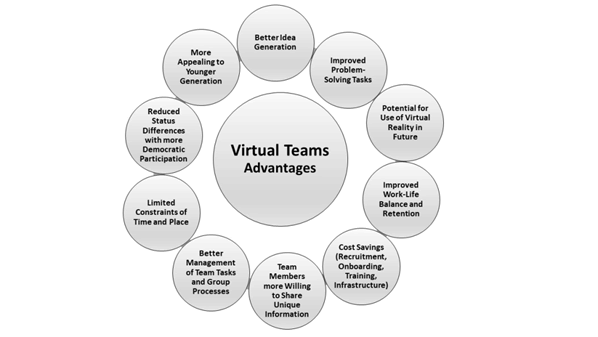
Virtual teams in general are superior for idea-generation, for more robust participation, better management of team tasks and group processes, problem-solving, and improved decision-making because of increased willingness of team members to share unique information, considerable cost-savings, increased productivity, having limited constraints in time and place, and with a greater appeal to the younger generation (Figure 2) [12]. Virtual teams also strengthen the emerging concept of the highly operational “decentralized model” in conventionally tiered institutions as endorsed by U.S. Army General Stanley McChrystal with “teams of teams” constructs emphasizing “decentralized autonomy, meritocracy, and sense of partnership” [26].
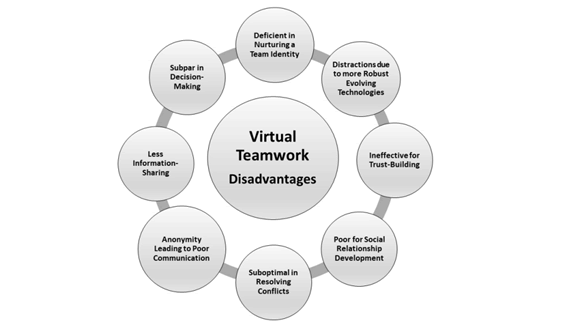
Virtual teams are inferior for information sharing, nurturing team identity, and trust-building, are subpar for decision-making and negotiation tasks, and may lead to social isolation. As alluded to previously, they also risk distraction due to evolving innovative technologies (Figure 3) [12]. The dominant challenges confronting virtual teams center around effective communication, building trust, and creating effective interpersonal and social relationships. A variety of team-building approaches have been proposed to facilitate teams in surmounting these shortcomings via training, better clarity of role, and more effective communication strategies. However, despite the many advantages and disadvantages, overall team performance (virtual versus conventional) often is reportedly similar for proficient teams. It is likely that the effectiveness of virtual teams will continue to improve in the future because of the increased use of technology for informal as well as social communication by numerous stakeholders.
Influence of COVID-19 pandemic on virtual teamwork
The COVID-19 pandemic and accompanying global crisis have affected many facets of our daily lives (e.g., financial services, media, education, etc.) including the mission(s) of AMIs. Employees of AMIs have had to adapt to the virtual teamwork environment and the new paradigm to circumvent lockdowns, secure childcare following daycare and school closures, and follow social distancing requirements. There has been an acceleration of the trend towards digital transformation during the pandemic with work being increasingly conducted remotely via phone, E-mail, instant messaging, and videoconferencing. The impact of this paradigm shift coupled with growing “work from home” movement that preceded the pandemic remains uncertain at this juncture. The value of virtual teamwork may be dubious if employees continue to be productive, reliable, and effective in a non-virtual context. Moreover, the important facets of building trust and conflict resolution without the benefit of gestures (body language, facial cues, hand signals, etc.) or direct social interaction with videoconferencing are unclear and warrant further investigation [25,27].
Conclusions and Future Directions
The COVID-19 pandemic has escalated the incipient momentum of virtual teamwork in fulfilling the mission(s) of AMIs. While the further course of the pandemic is difficult to envisage, it is plausible that virtual teamwork will replace conventional methodologies such as in-person meetings, lectures, and conferences and become increasingly common in our repertoire with stakeholders adjusting to emerging newer communication technologies with iterative refinements. Interfacing with virtual reality and machine learning in the not-too-distant future is an emerging certainty. Meanwhile, perhaps a “hybrid” of in-person and virtual teamwork is a more predictable reality and will become the norm in the foreseeable future. It is prudent for stakeholders to continually appraise, recalibrate, adapt and adjust to this evolutionary “new world order” in communication in fulfilling our mission(s) in AMIs.
References
- Fleishon HB, Itri JN, Boland GW, Duszak Jr R (2017) Academic medical centers and community hospitals integration: Trends and strategies. J Am Coll Radiol 14: 45-51.
[Crossref], [Google Scholar], [Indexed]
- Chari R, O'Hanlon C, Chen P, Leuschner K, Nelson C (2018) Governing academic medical center systems: Evaluating and choosing among alternative governance approaches. Acad Med 93:192-198.
[Crossref], [Google Scholar], [Indexed]
- Guzick DS, Wilson DE (2018) Governance of academic medical centers is indeed a complex and unique operation. Acad Med 93:154-156.
[Crossref], [Google Scholar], [Indexed]
- Pellegrini Jr VD, Guzick DS, Wilson DE, Evarts CM (2019) Governance of academic health centers and systems: A conceptual framework for analysis. Acad Med 94: 12-16.
[Crossref], [Google Scholar], [Indexed]
- Bhardwaj A (2017) Alignment between physicians and hospital administrators: Historical perspective and future directions. Hosp Pract 45: 81-87.
[Crossref], [Google Scholar], [Indexed]
- Bhardwaj A (2019) What's new in academic International medicine? The evolving terrain of American Academic medicine. Int J Acad Med 5:85-92.
[Crossref], [Google Scholar]
- Marks L (2020) The landscape of academic medicine and health care in the United States. Pharos pp: 2-8.
[Crossref], [Google Scholar]
- Bhardwaj A (2022) Organizational culture and effective leadership in academic medical institutions. J Healthcare Leadership 14 25–30.
[Crossref], [Google Scholar], [Indexed]
- Azad MB, Rodriguez N (2021) Team science: Defining and achieving success. Clin Invest Med 44: E1-4.
[Crossref], [Google Scholar], [Indexed]
- Pollock DM, Pollock JS (2015) Mentoring for collaborations and team science. Physiologist 58:279, 282-4.
[Crossref], [Google Scholar], [Indexed]
- Taylor F (1923) The principles of scientific management. New York, NY: Harper.
- Levi D (2017) Group dynamics for teams. 5th Edition. Sage publications, Thousand Oaks, CA.
- Mayo E (1933) The human problems of an industrial civilization. Cambridge, MA: Harvard University Press.
- Zigurs I (2003) Leadership in virtual teams. Oxymoron or opportunity. Organizational Dynamics 31, 4; 339-351.
[Crossref], [Google Scholar], [Indexed]
- Tannenbaum S, Mathieu J, Salas E, Cohen D (2012) Teams are changing: Are research and practice evolving fast enough? Industrial and Organizational Psychology 5(1), 2–24.
[Crossref], [Google Scholar], [Indexed]
- Rosen MA, Granados DD, Dietz AS, Benishek LE, Thompson D, et al. (2018) Teamwork in healthcare: Key discoveries enabling safer, high-quality care. Am Psychol 73: 433-450.
[Crossref], [Google Scholar], [Indexed]
- Institute of Medicine (IOM) (2001) Crossing the quality chasm: A new health system for the 21st century. Washington, D.C: National academy press.
[Crossref], [Google Scholar], [Indexed]
- Stasha M. The state of healthcare industry-Statistics for 2022.
- Shim JP, Warkentin M, Courtney JF, Power DJ, Sharda R, et al. (2002) Past, present, and future of decision support technology. Decision Support Systems 33:111-126.
[Crossref], [Google Scholar]
- Duarte D, Snyder N (2006) Mastering virtual teams. 3rd Edition. San Francisco: Jossey-Bass.
- Shigekawa E, Fix M, Corbett G, Roby DH, Coffman J (2018) The current state of telehealth evidence: A raid review. Health Affairs 37: 1975-1982.
[Crossref], [Google Scholar], [Indexed]
- Doraiswamy S, Abraham A, Mamtani R, Cheema S (2020) Use of telehealth during the COVID-19 pandemic: Scoping review. J Med Internet 22: e24087.
[Crossref], [Google Scholar], [Indexed]
- Crites GE, Berry A, Hall E, Kay D, Khalil MK, et al. (2020) Applying multiple frameworks to establish effective virtual collaborative teams in academia: A review and recommendations. Med Edu Online 25: 1-10.
[Crossref], [Google Scholar], [Indexed]
- Fowler T, Phillips S, Patel S, Ruggiero K, Ragucci K, et al. (2018) Virtual interprofessional learning. J Nurs Edc 57: 668-674.
[Crossref], [Google Scholar], [Indexed]
- Barry DM, Kanematsu H, Ogawa N, McGrath P (2021) Technologies for teaching during a pandemic. Procedia Computer Science 192:1583-1590.
[Crossref], [Google Scholar], [Indexed]
- McChrystal GS, Collins T, Silverman D, Fussell C (2015) Team of teams: New rules of engagement for a complex world. Penguin.
- Agarwal S, Ferdousi S, John M, Nalven A, Stahl T. Effective leadership in virtual teams during the COVID-19 pandemic. ETM Student Projects.
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences